Xbow System Lectures
The Four Tool Boxes for Class II Treatment
Informed consent is the legal responsibility of the orthodontist to explain the pros and cons of all possible treatment options, and to help the patient and their family determine which option is best for them.
One type of Class II bite problem is when there is a horizontal gap between the upper and lower front teeth, also known as excess overjet. 53% of the population has a Class II bite with an overjet greater than 3mm. 15% of the population has a moderate to severe Class II bite problem with 5mm or more of overjet.
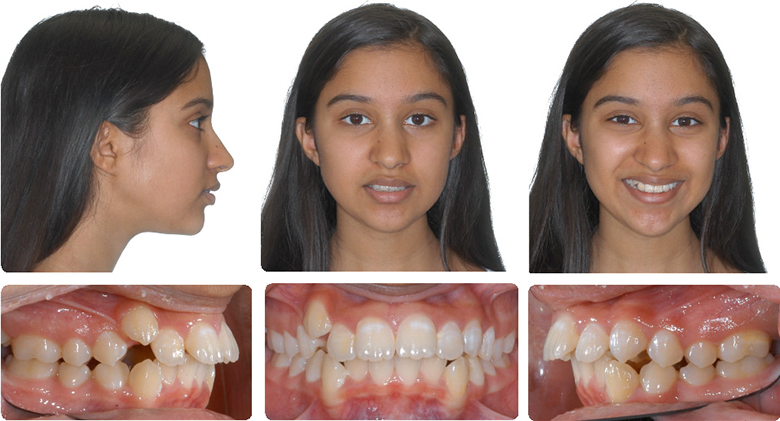
The cause of excess overjet is usually a small or receding lower jaw and chin, but there can also be a protrusion of the upper front teeth.
The Four Tool Boxes Analogy
In Dr. Higgins’ office there are four different options for the treatment of a Class II bite problem.
- The Surgery Tool Box
Braces to straighten the teeth and place the front teeth and lips in an ideal position, followed by surgery to lengthen the lower jaw, is often the best option to correct the bite and balance the appearance of the nose, lips, and chin. - The Traditional Treatment Tool Box
Braces and the extraction of two upper teeth are used to retract or “pull back” the upper front teeth to correct the bite and camouflage the small or receding lower jaw and chin. We call this Class II compensation. This is a good choice if the upper front teeth are crowded or protruding. The down side of this treatment is it can result in loss of upper lip fullness. - The Crossbow Tool Box
The Crossbow Class II Corrector shares the correction between the upper and lower teeth. It moves upper teeth back and lower teeth forward. This minimizes the retraction of the upper front teeth and upper lip. This is another type of Class II compensation. It is meant to be used in a growing patient, and works best if the patient is in their growth spurt. The down side is that it still moves the upper lip back, just not as much as traditional extraction treatment. It also moves the lower lip forward, which can be a plus or a minus. Even if surgery is the best option, most patients still choose the Crossbow Tool Box, to avoid surgery and extractions. Sometimes the Crossbow is not a good option, especially if the patient is finished growing, or if the lower front teeth are crowded or protruded, or if the lower lip is protruded. - The Class II Elastic Tool Box
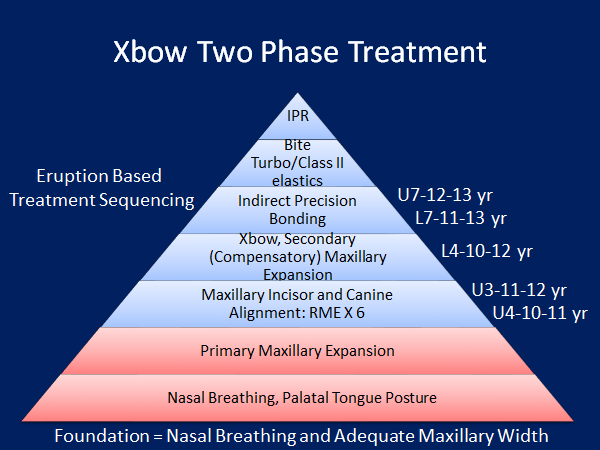
Braces or Aligners combined with Class II elastics is probably the most common treatment in use today. It is popular because it is the least expensive. It requires the least effort by the orthodontist, but the most effort by the patient. Simply put, if the patient does not wear the elastics, they end up with straight teeth but with a remaining bite problem, or excess overjet. If the patient wears the elastics well, the result may be similar to the Crossbow, with two exceptions. One, Class II elastics have a tendency to pull the upper front teeth down, making a gummy smile worse. Two, when used with aligners Class II elastics may push the lower front teeth out of the bone, exposing the roots. The other problem with aligners is they require much more patient cooperation than braces, and there are many tooth movements that aligners don’t do well or not at all. This is why the best orthodontists that use aligners use them in conjunction with braces. Braces are still used to do the “heavy lifting”.The general rule is it is best to choose a treatment plan that decreases elastic wear and patient cooperation because poor cooperation can increase the length of treatment. Long treatment time increases the risk of root resorption (root shortening) and decalcification (white spot lesions or cavities).Dr. Higgins has developed systems that decrease the time in braces to 12 to 18 months, even for extraction treatment. This includes indirect (precision) bonding of brackets (braces). He also uses a low force technique with a smaller bracket slot and smaller wires compared to the majority of orthodontists. This is more comfortable for the patients and may result in less root resorption.The Crossbow appliance is part of Dr. Higgins’ “foundation building” philosophy of treatment. It is based on the principle of waiting until all teeth have erupted, including second molars, before placing full braces. “Building the foundation” includes establishing a normal upper jaw width with an expander (RME), correcting a Class II bite with a Crossbow appliance, and opening space for upper canine teeth with partial braces (RME X 6).
Dr. Higgins is a clinical assistant professor at the University of British Columbia. More information can be found on the Crossbow website at www.crossboworthodontic.com.
Foundation Rules
- Treat the biggest problem first.
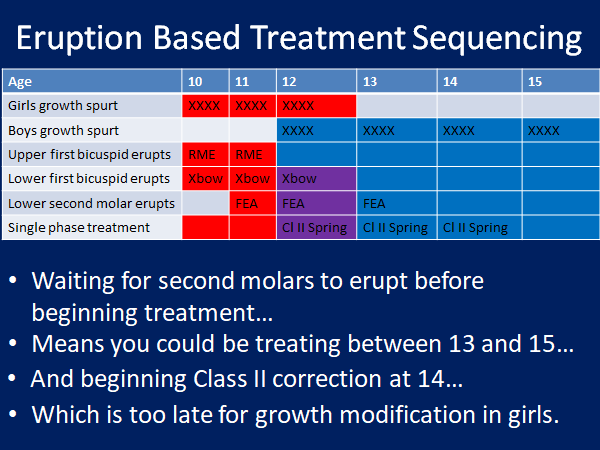
- Sequence treatment based on the eruption.
- Begin with primary maxillary expansion if there is a posterior crossbite or if the maxillary lateral incisors are impacted. These teeth erupt at 8 to 9 years old on average.
- Time first phase treatment when the first bicuspids are erupting at 10 to 12 years old to make room for the erupting maxillary canines at 11 to 12 years. This will reduce the incidence of impacted maxillary canines.
- Don't place full edgewise appliances until the second molars have erupted or you will prolong your second phase treatment and increase decalcification and root resorption.
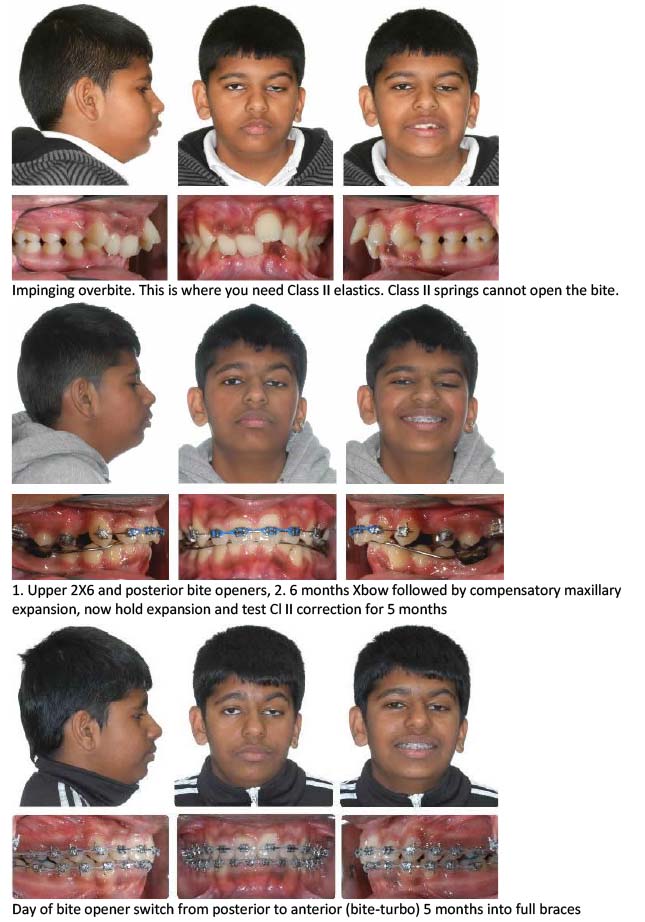
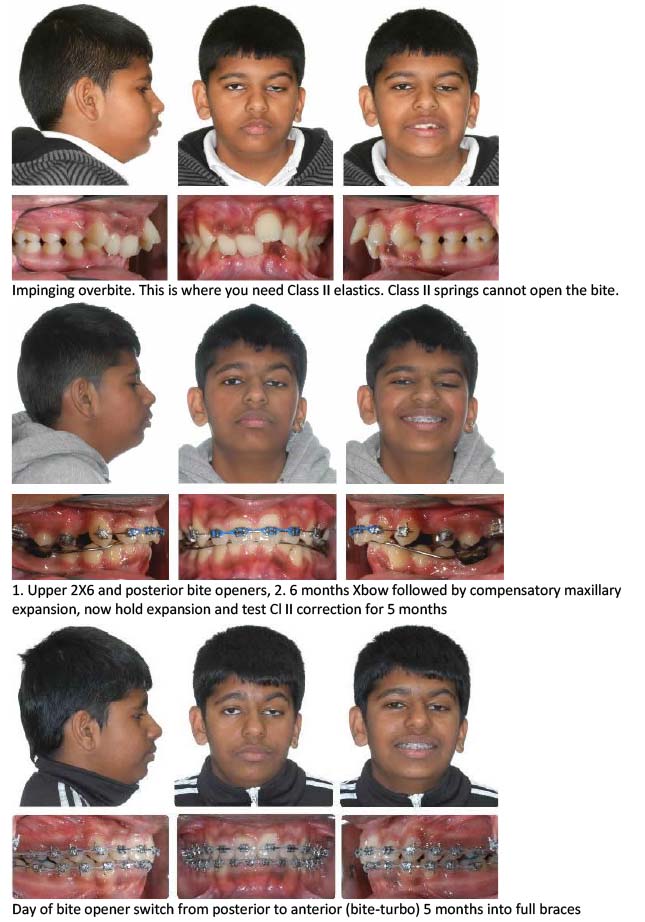
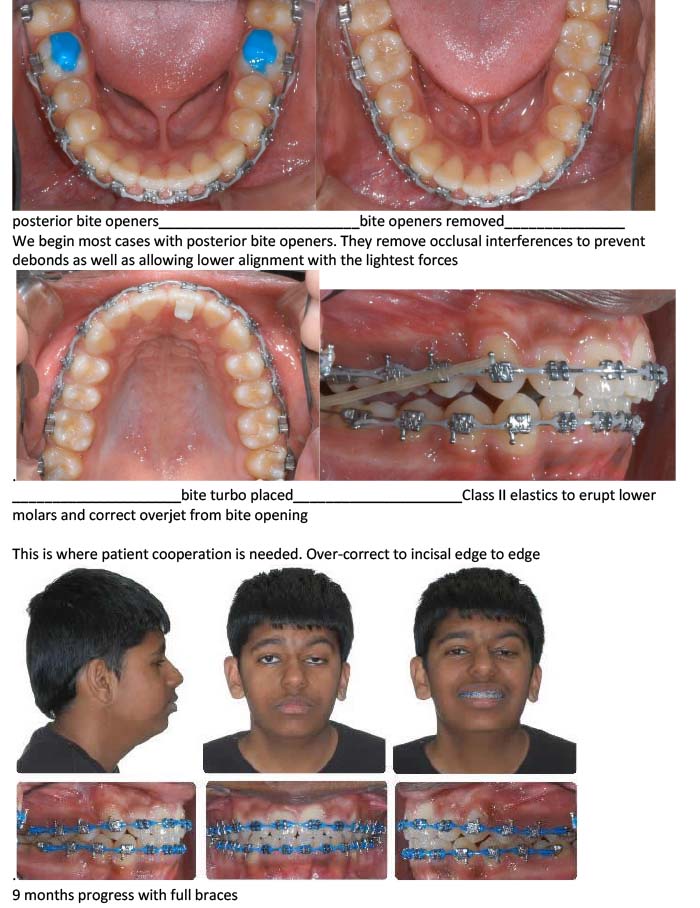
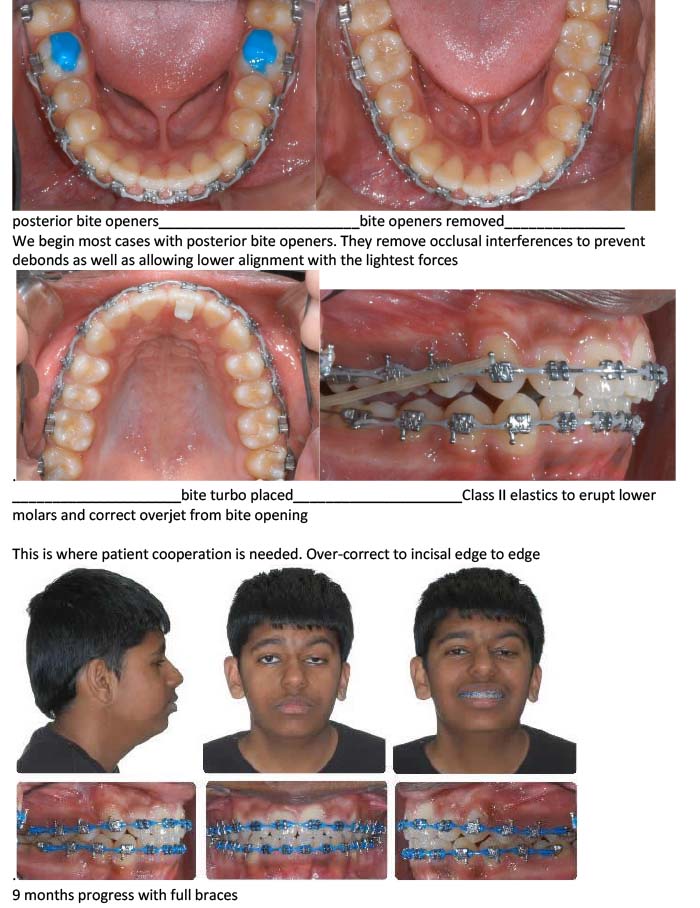
- Save cooperation with Class II elastics in deep overbite cases until you are in full-size stainless steel arch wires and the overjet is reduced enough to place a bite turbo.
- Try to postpone IPR (interproximal reduction) of the incisors until all spaces are closed, the buccal occlusion is Class I, and the overbite and overjet are corrected. The goal is to create long, flat interproximal contacts without black triangles keeping in mind not to create a tooth mass discrepancy. This is impossible to do with early IPR.
- Always go back to the foundation base during treatment to make sure the patient can breathe through the nose, keep the tongue on the anterior palate, swallow without a tongue thrust, and keep the lips together at rest, if possible.
- Initial, posterior Crossbite, & Anterior Crowding
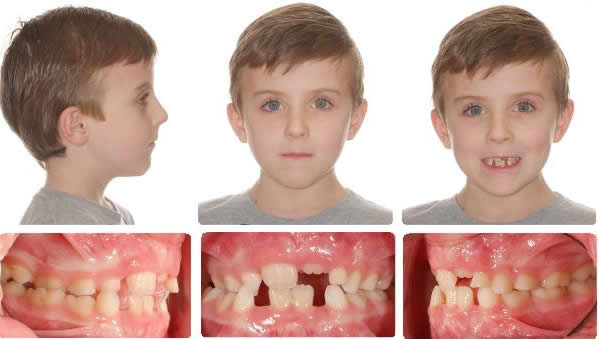
Initial, posterior crossbite and anterior crowding

4 Years After Maxillary Expansion
Taken 2 Years after Xbow Removal

Initial

4 Years After Maxillary Expansion

2 Years After Xbow, No Braces Used
RME X 6: Combining Maxillary Expansion & Anterior Alignment to Establish the Maxillary Foundation
The Xbow System is based on treating to an ideal maxillary arch form and width. Combining anterior alignment with Rapid Maxillary Expansion is more effective than archwire expansion by itself.

RME X 6 appliance with 12 mm Dentaurum "Variety" expansion screw, 100-gram shorty open coil nickel-titanium springs to open space for canines, occlusal rests for second molars. Mini tubes are welded to the first bicuspid bands in such a way as to control the movement of the canine and incisor occlusal plane.

After 6 Months RME X 6

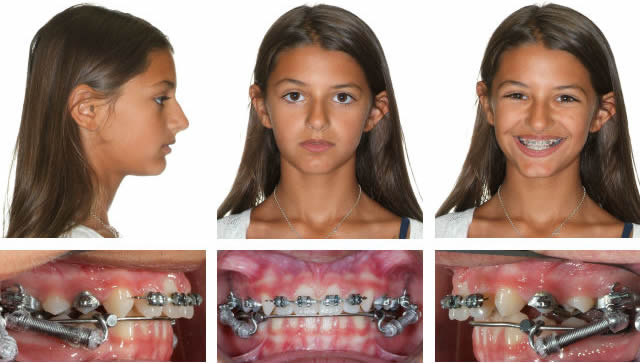
RME X 4/Xbow with Mesial Hookup & Upper Incisor Segment


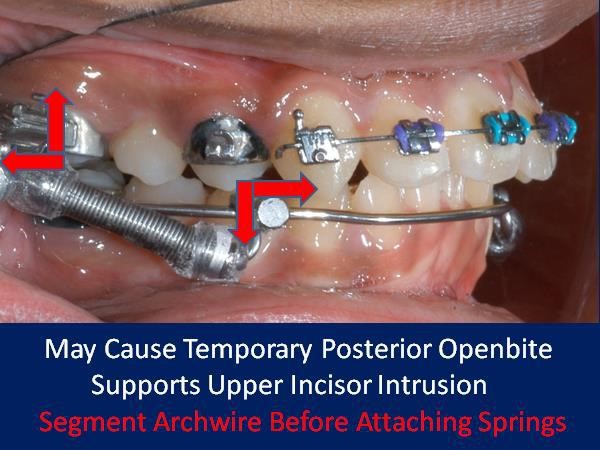
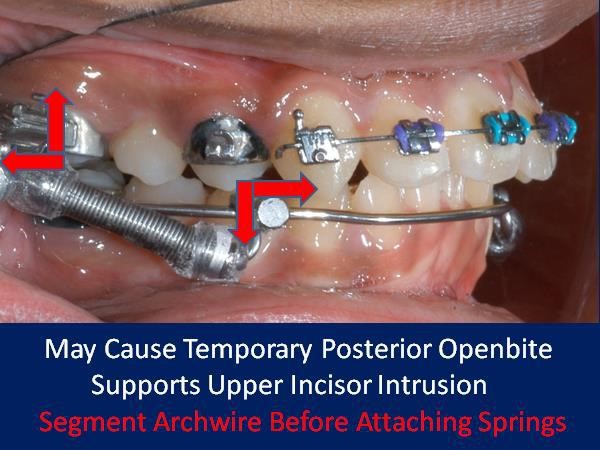
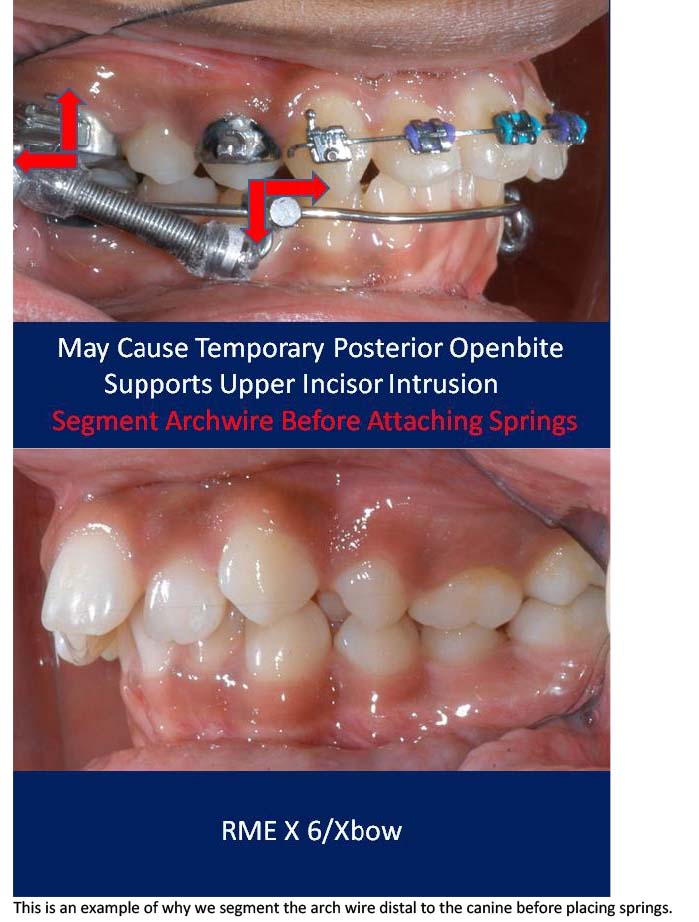
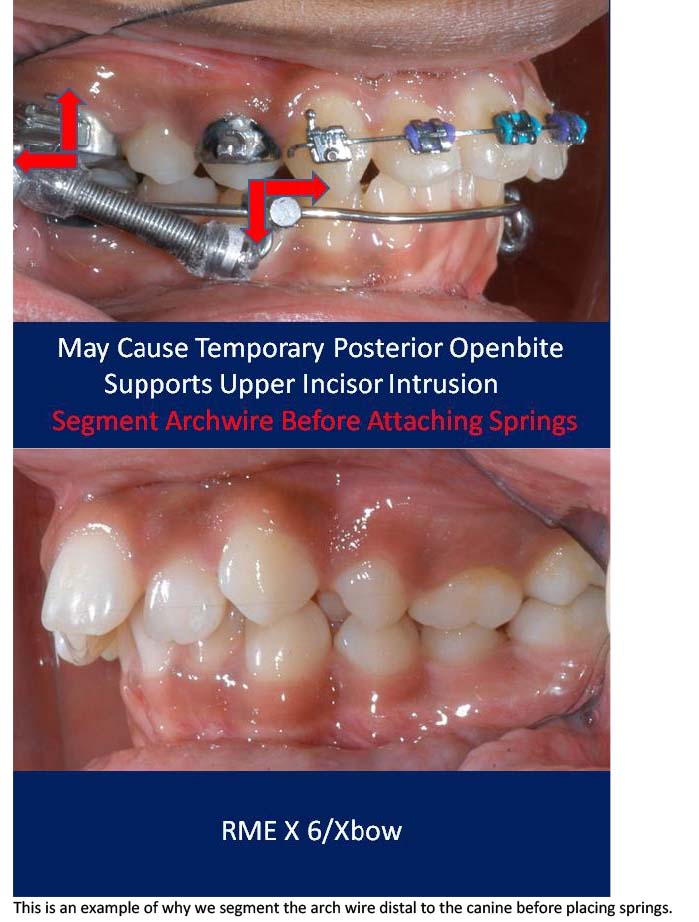
RME X 6/Xbow appliance with mesial hookup and archwire segmented distal to canines before Class II spring attachment.

RME X 6/Xbow after Class II springs removed after over-correction of Class II, shows spring side effect of buccal segment occlusal plane tipping down in front. If archwire was not segmented the anterior teeth would have been extruded and tipped lingually into crossbite.
RME X 6/Xbow Cases Treated by Dr. Higgins

Initial
After Upper Incisor Alignment, Day of Xbow Insertion

After 3 Months of Xbow Followed by Compensatory Maxillary Expansion, Now Will Retain Expansion, & Test Class II Correction for 5 Months Before Removing Appliances

Ready for Phase 2 Braces

8 Months Braces

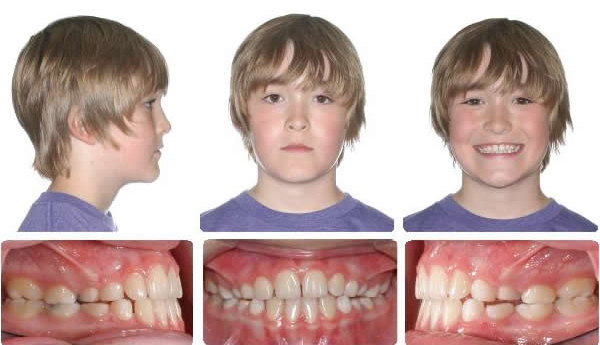
This high angle patient presented with a half cusp Class II bicuspid relationship and a bicuspid openbite on the right side.

After RME X 6/Xbow Showing Buccal Segment Over-Correction. Once the Anteriors Were Aligned the Triple "L" Arch & Springs Were Placed. The springs were on for 3 months before compensatory maxillary expansion was started. The expansion was retained for 5 months before the appliance was removed.

10 Months Full Braces

This next patient is an example of upper anterior crowding where the molars are Class I but the bicuspids are a half cusp Class II and the upper canines are blocked out and a full cusp Class II. This required an RME X 6 appliance to align the anteriors before the placement of the Triple "L" Arch and springs.

Initial

After upper alignment and Xbow correction to Class I bicuspid. Leave springs on to over-correct.

Day of spring removal after over-correction. Springs were on for 4 months.

RME X 6 with upper second molar mini tubes on bicuspid bands. 016X.025 SS anterior segment (Use active retraction of upper incisors with a continuous archwire as little as possible to avoid root resorption.)

Day of appliance removal and placement of upper Essix retainer, Ready for indirect bonding of full braces.

7 Months Full Braces

Initial

RME X 6v-v2. 4 Months Xbow, Ready for Maxillary Expansion

11 Months After Spring Removal, Full Braces Have Not Been Used
Class III Malocclusion
The RME X 6 is used with Class III malocclusions when maxillary expansion and/or upper incisor proclination is indicated. A reverse pull headgear (protraction face mask) can be added by attaching elastics to the first bicuspid hooks or the long ends of the archwire distal to the bicuspid tubes.


Progress

End of Phase One

RME to open space for upper lateral incisors. RME X 4 and bonded posterior bite blocks to rotate mandible down and back and then procline upper incisors.
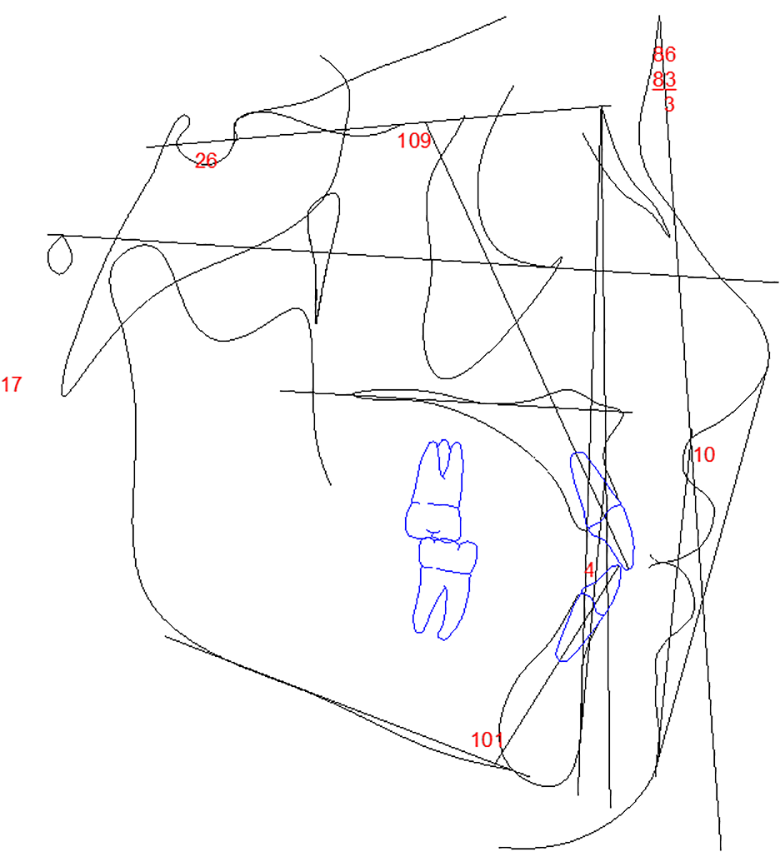
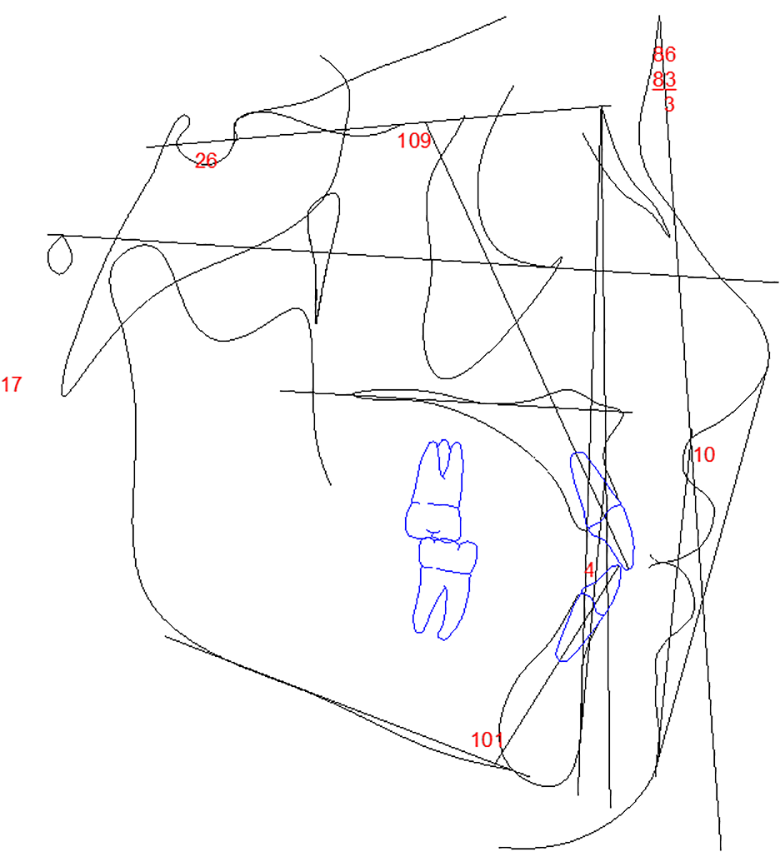
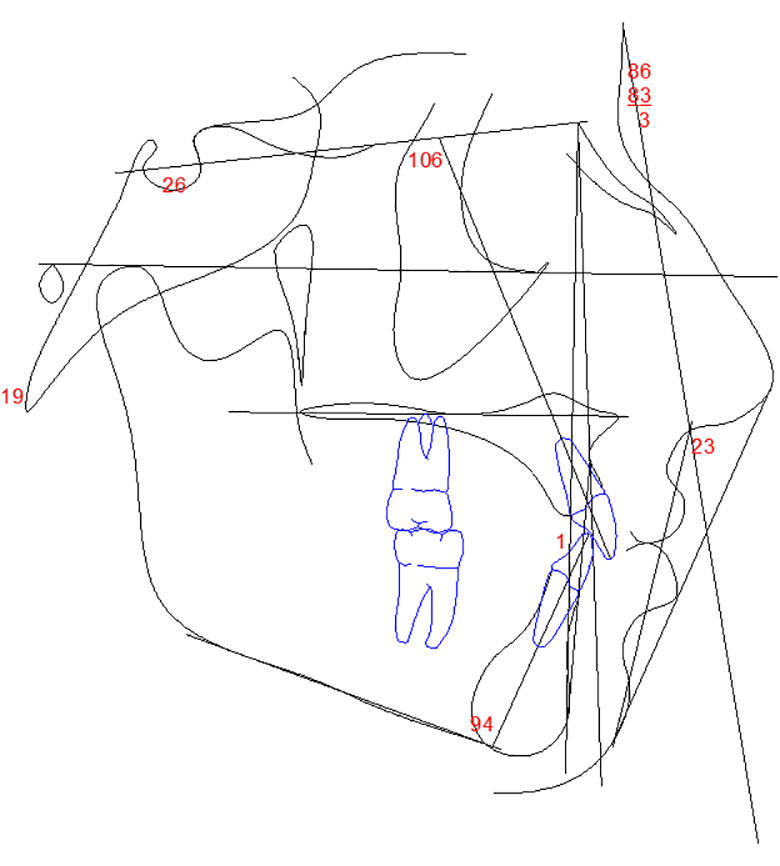
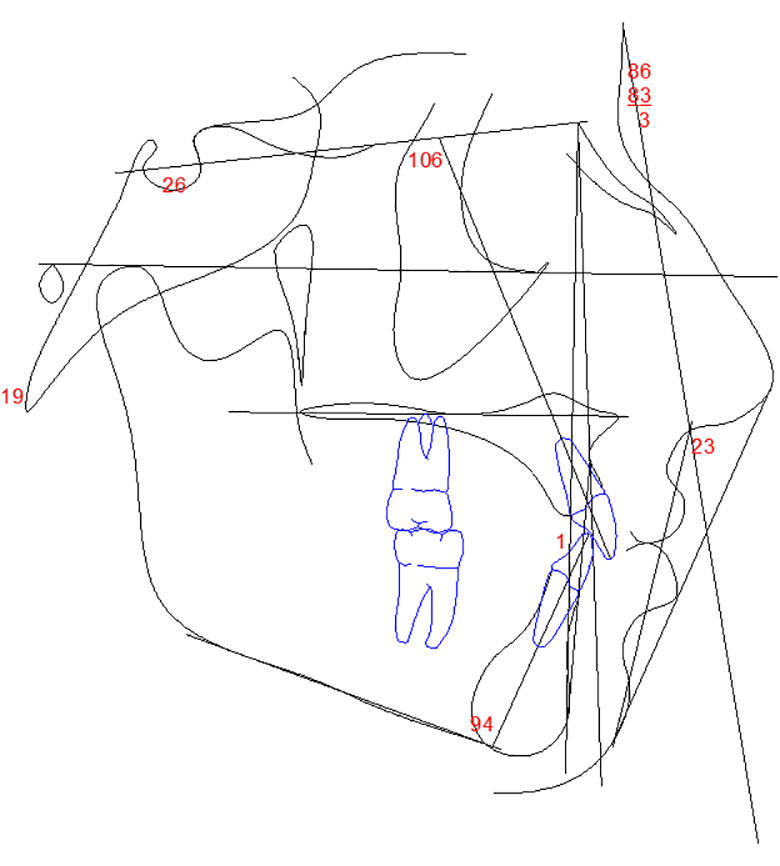
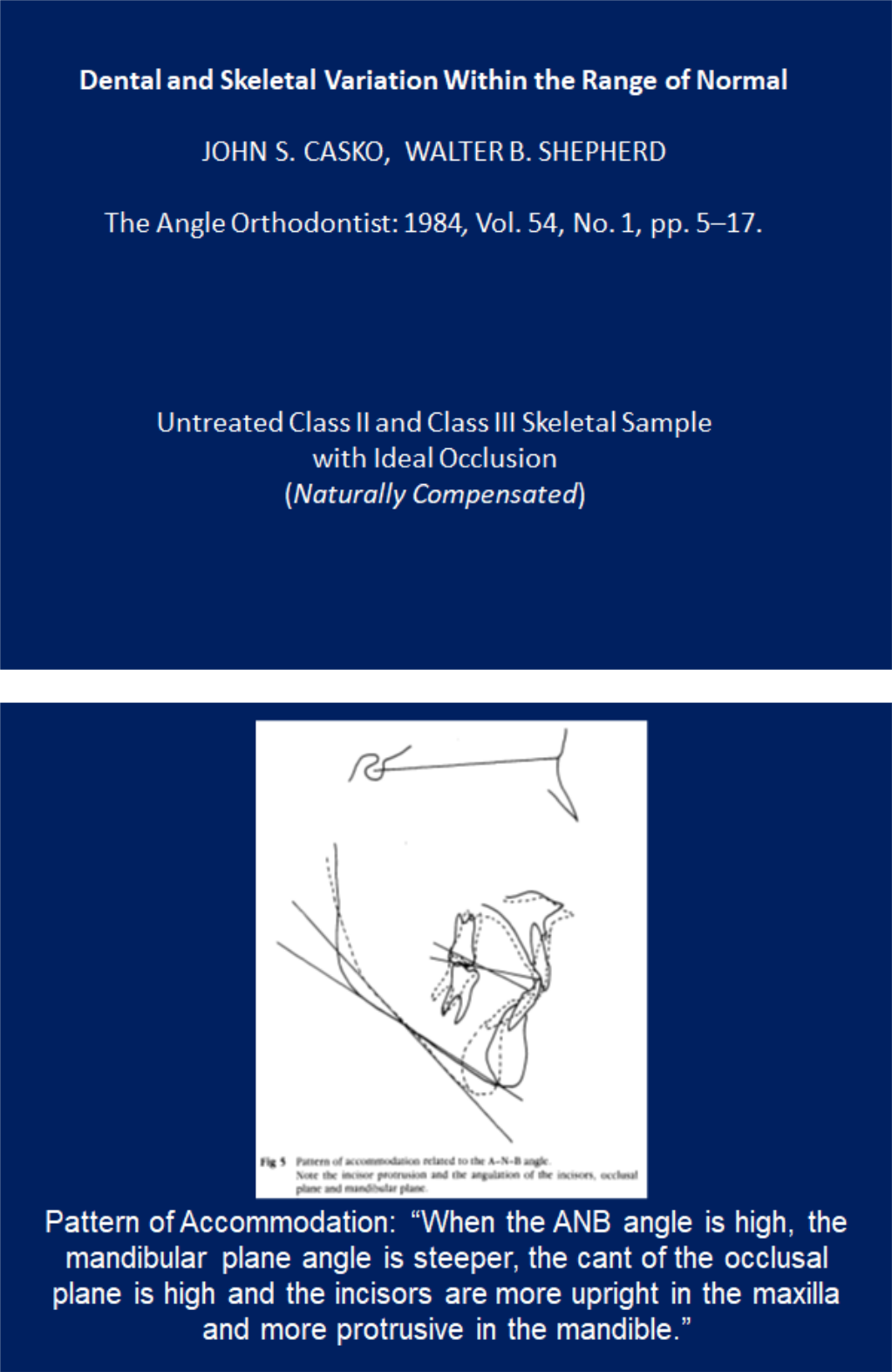
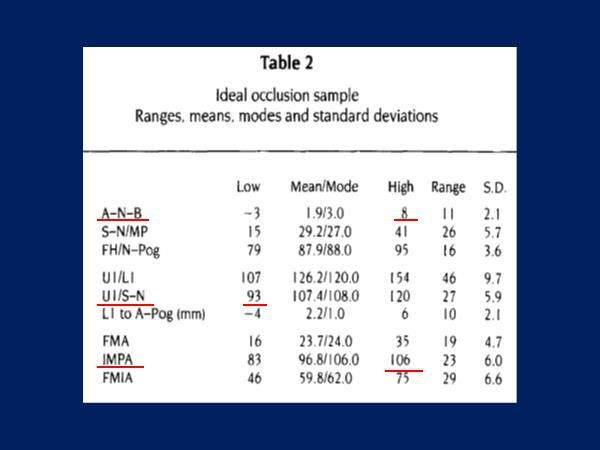
Class II Compensation Compared to Class III Compensation
In Dr. Casko's untreated ideal occlusion study where the ANB angle was -3 degrees, the lower incisor was compensated back to 83 degrees while the upper incisor was compensated out to 120 degrees. In order to prevent Class III surgery orthodontists will procline upper incisors out to 120 degrees without a second thought, which is 18 degrees past the norm. The same orthodontists may criticize a lower incisor proclined to 106 degrees in a Class II patient, which is only 10 degrees past the norm.
Same patient as above, flipped lower to upper. Why should a Class II be treated differently than a Class III?





Proclining Upper Incisors to Avoid Cl III Surgery



Initial

Progress

Final

Initial to Final
Maxillary expansion only to open space for the upper lateral incisors, mandible rotated down and back, correcting the anterior crossbite.


Initial

Maxillary expansion and protraction headgear for 4 months followed by 2 months settling.

9 Months Braces

Initial
6 Months maxillary expansion and protraction facemask, photos taken one month after appliance removal, note mandibular asymmetry, Class II right, Class III left.


RME & Protraction Facemask
Combination Active Anteriors and Passive Posteriors (CAAPP) Orthodontic Skating: Sliding with Control

CAAPP with G&H Agility PSL brackets on canines and bicuspids.
CAAPP combines incisor control with ligated twin brackets and decreased resistance to sliding with passive self-ligating brackets on canines and bicuspids, creating a "long buccal tube." Ligated incisors also give young patients what they ask for, colored ligatures.
.018 inch bracket slot, .018X.025 inch archwire, Carriere passive self-ligating bracket sliding on archwire with Innovation active self-ligating brackets acting as end stops.
.018 inch bracket slot, .016X.022 inch archwire, Lotus Plus passive self-ligating bracket sliding on archwire with Lotus Plus interactive self-ligating brackets acting as end stops.
In a group of 145 consecutively debonded patients from the author's practice, the average treatment time from bonding to debonding was 16 months. 78% of the patients had an average treatment time of 13.4 months.
The part of treatment that the orthodontist has control over (other than the treatment plan) is Alignment and Space Closure (ASC). The patient has control over elastic wear to coordinate the arches and finish the occlusion. In a group of 42 consecutively treated patients where 34 were non-extraction and 8 were extraction cases, ASC took an average of 9 months to complete for the non-extraction group and 11 months for the extraction group.
CAAPP TwinLok 1997
I was asked to test the .018 version of the TwinLok passive self-ligating bracket in 1997. The result was the incomplete alignment of the lower incisors and a lack of torque control of the upper incisors. This was due to the play between the archwire and the slot. The slot depth was .030 inches. This was done to accommodate the anterior curvature of the archwire and still allow the clips to close.
The low resistance to sliding in the canine and bicuspid brackets was an advantage. It was easier to close space, retract canines, and advance incisors.
I changed the TwinLok brackets to ligated twins on the incisors and traded free sliding for control, creating a hybrid system similar to Dr. Gianelly's bi-metric technique.
Ligating the archwire to the incisor bracket slots' base allows the maximum deflection and activation of the lightest archwires and the fastest incisor alignment with the lightest forces.
Proponents of passive self-ligating brackets thought that ligated incisor brackets would slow down anterior alignment and require heavier forces to overcome resistance to sliding. The following examples show that this is not the case.

Initial placement of .012 niti

After 2 Months, Day of Change to .018 Niti to Lower Second Molars

Initial

After 2 months with .012 niti, day of .018 niti placement.

After 1 month of .018 niti, day of .014X.025 niti placement.

Initial placement of .012 niti and elastic chain to canine

2 months with .012 niti and elastic chain to canine, day of change to .014X.025 niti.
The following is a bicuspid extraction case showing rapid alignment with CAAPP.

Initial

Indirect bonding, Extractions, .012 Niti Archwires Placed

3 Weeks Later: Begin Light Elastic Chain under the .012 Niti Archwire

6 Weeks Later: Day of Change to .018 Niti Archwires

4 Weeks Later: 13 Weeks Total for Initial Alignment. Day of Change to .014X.025 Niti Archwires
I am currently using the Lotus Plus DS Hybrid self-ligating bracket system which is active on incisors and passive on canines and bicuspids. I use the MBT prescription in a .018-inch slot. The slot tolerances are tight and we find it difficult sometimes to close the clips when using .017X.025-inch archwires. Presently the archwire progression we are using is .012-inch niti, followed by .014-inch niti (if necessary), followed by .018-inch niti to the second molars, followed by .016X.022-inch niti, and finally, .017X.022-inch heat-treated stainless-steel archwires. Final adjustments are done in .016X.022-inch beta titanium.
When I started with Dr. Michael Wainwright he was using two archwires, .016-inch niti followed by .016X.022-inch stainless steel. I was amazed at the simplicity and efficiency compared to the segmented arch technique that we were both taught at Indiana University. I am now using more archwires in the progression but I am convinced I am using the lightest forces which will decrease root resorption and is more comfortable for my patients.


"C" Clip, SS Passive, Lotus Passive, and Lotus Interactive
The Lotus Interactive niti clip seats the archwire in the floor of the slot with a force that is perpendicular to the slot, unlike a "C" Clip.

Four arch sizes=three pairs (Small, Medium, Large)
To purchase these wires in most sizes contact Mark James at G and H Orthodontics.
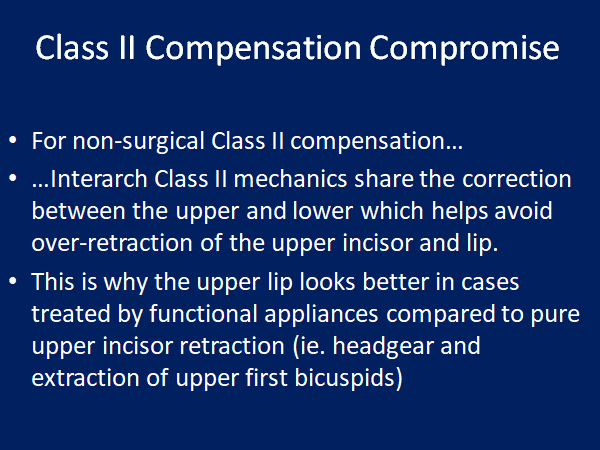
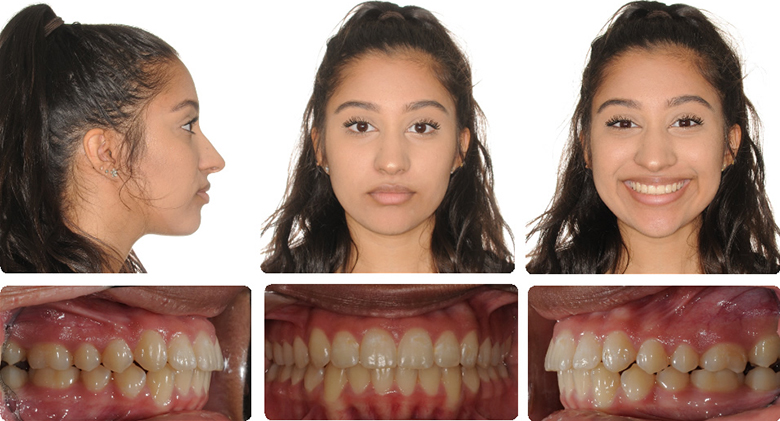
The Class II Compensation Compromise: Preserving the Upper Lip


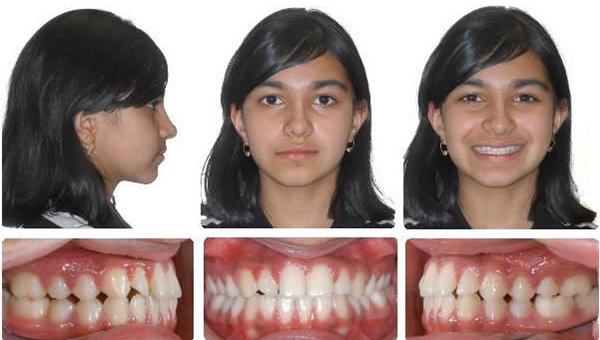
Before

After, treated non-extraction with phase one bionator followed by full edgewise and cervical headgear, care taken not to procline lower incisors.

Same patient showing opening of naso-labial angle due to upper incisor retraction.
This patient was the one that made me think more about preserving the upper lip. I read everything I could find in the orthodontic, surgery, and periodontal literature. My study club invited Dr. Clark to speak to us about Twin Blocks. I began using Twin Blocks but changed to the four crown cantilever Herbst appliance. The temporary over-proclination of lower incisors surprised me at first, but I did not see a gingival recession. Sharing the correction between the upper and lower resulted in less upper incisor and upper lip retraction.
As an orthodontic student in 1979 we were taught that our tool for a Class II malocclusion was orthodontic retraction and every problem was a protrusion.
Our toolbox had headgear and upper bicuspid extraction in it. In an emergency we could pull the red handle and use Class II elastics, but only if the lower incisors were retroclined or if we also extracted lower bicuspids. We looked at the models and the hard tissue ceph measurements.
For years I have been looking at the face as the most important determinant of which treatment I should recommend. For Class II patients this often means I will recommend jaw surgery as the best treatment. If the patient declines surgery I tell them treatment will involve dental compensation for their underlying jaw problem and that a compromise will involve a certain amount of upper incisor and upper lip retraction.
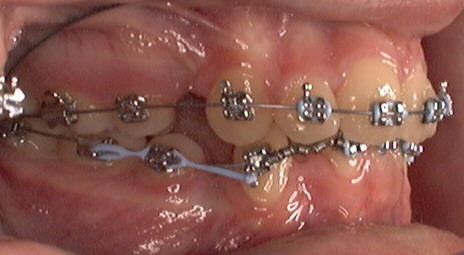
To minimize the retraction, Xbow shares the correction with the lower arch. This means lower incisor proclination and pemanent retention.
Xbow proclines lower incisors 3 degrees on average after a short period of over-proclination and rebound uprighting. In an unpublished study at the U of Alberta on 172 consecutively treated Xbow patients, the average lower incisor started at 99 degrees and ended up at 102.
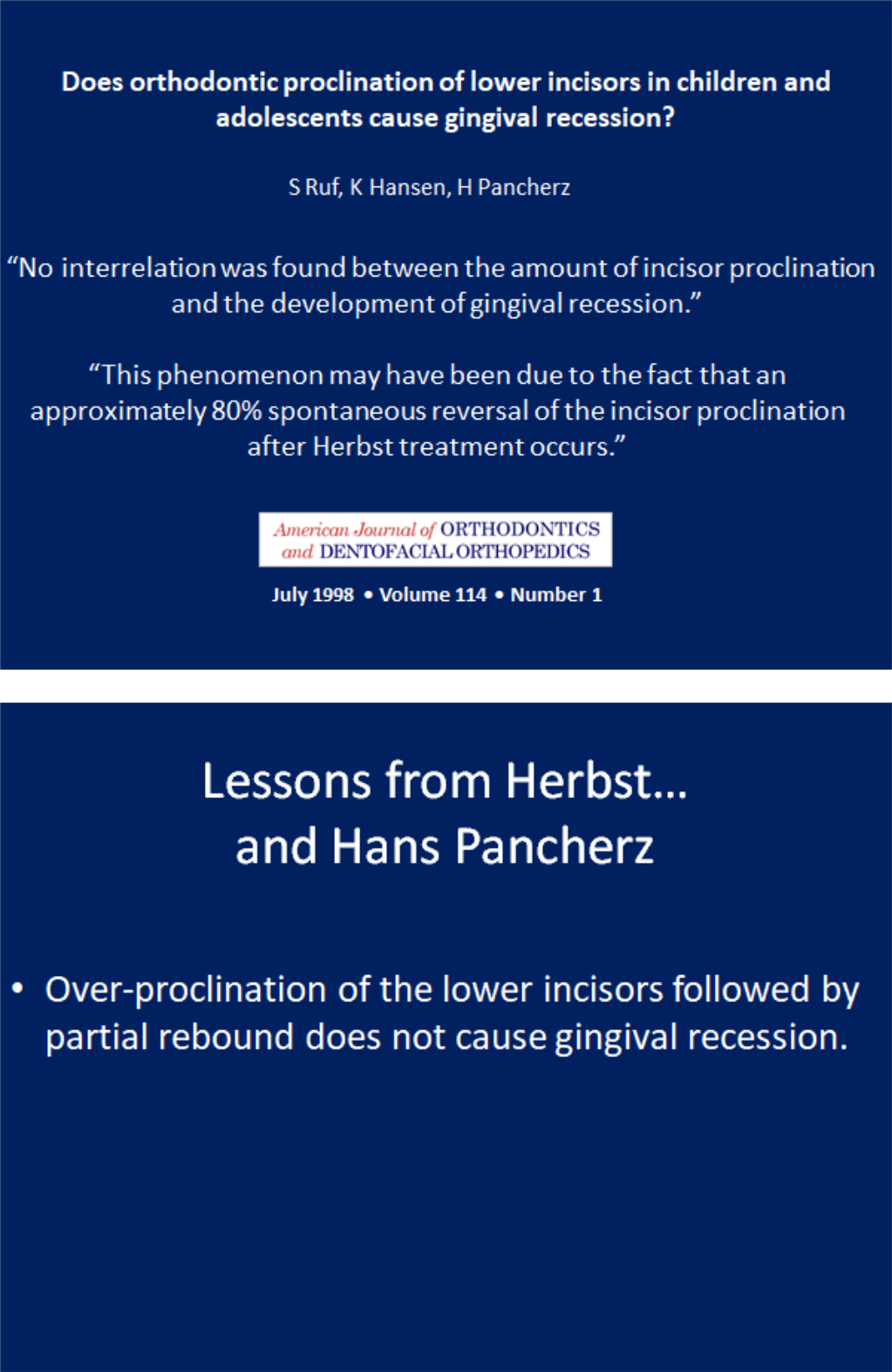
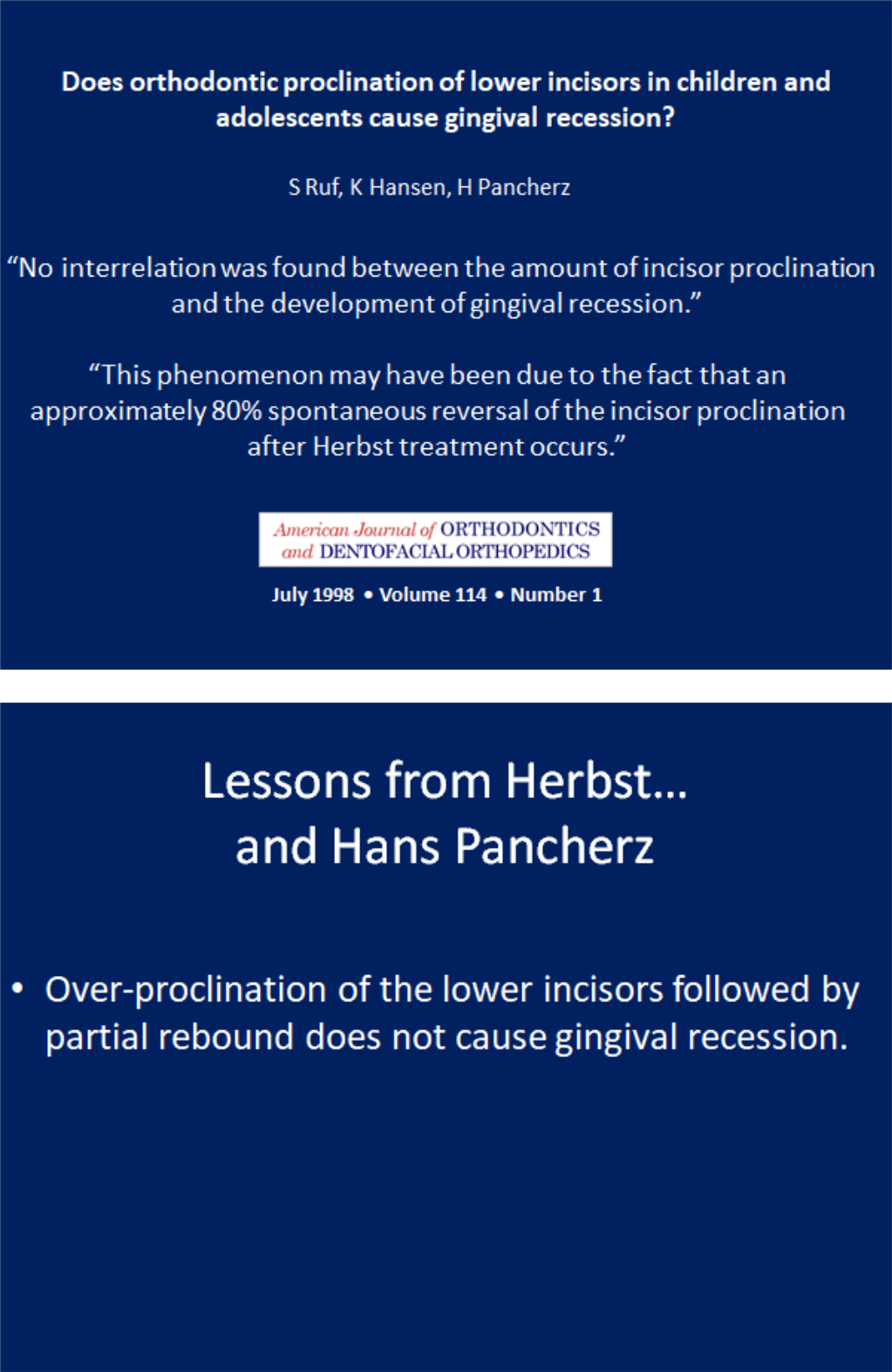
The literature is very clear. Lower incisor proclination does not cause gingival recession in healthy periodontium.
The literature is also very clear that all inter-arch Class II appliances procline the lower incisors a similar amount, even functional appliances. The non-edgewise Herbst appliance is capable of temporary over-proclination of the lower incisors similar to Xbow. This same over-correction is why the results are stable, and why phase two is shorter.
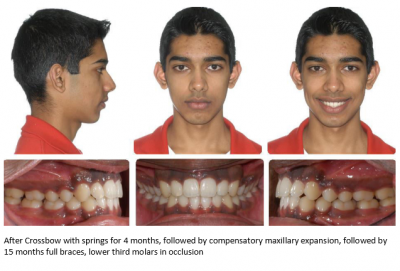
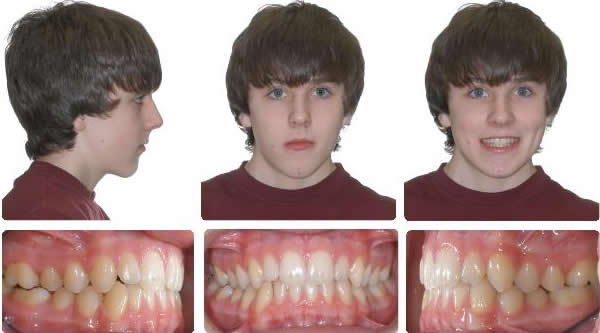
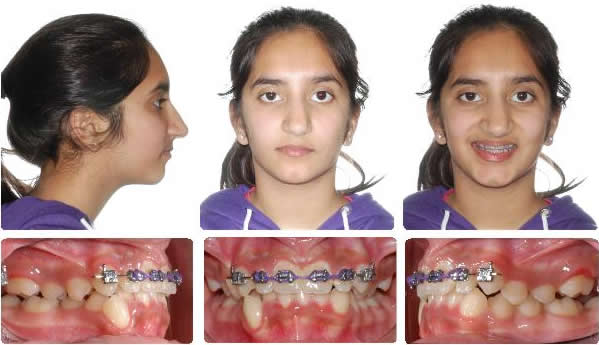
Xbow two phase non-extraction treatment to preserve the upper lip
Initial (I was the second opinion. Initial opinion was the extraction of four bicuspids and braces.Instead, I treated non-extraction with Xbow two phase treatment)
1. Xbow 2. RME 3. FEA

The Xbow system for Class II compensation is based on building the maxillary foundation for ideal treatment as if we were proceeding with jaw surgery. After maxillary expansion and upper anterior alignment, instead of proceeding with full braces and jaw surgery, we use the Xbow appliance to share the correction between both arches to minimize retracting the upper incisors and upper lip, compared to headgear or upper extractions.

Initial, Class II elastics should be minimized due to the gingival display

1. RME X 6 to intrude incisors 2. Xbow (springs for 2 months, intrusive springs support incisor intrusion)

14 months full braces


Upper lip preservation with a convex profile and obtuse naso-labial angle, non-extraction in a crowded Class II deep overbite patient



Initial

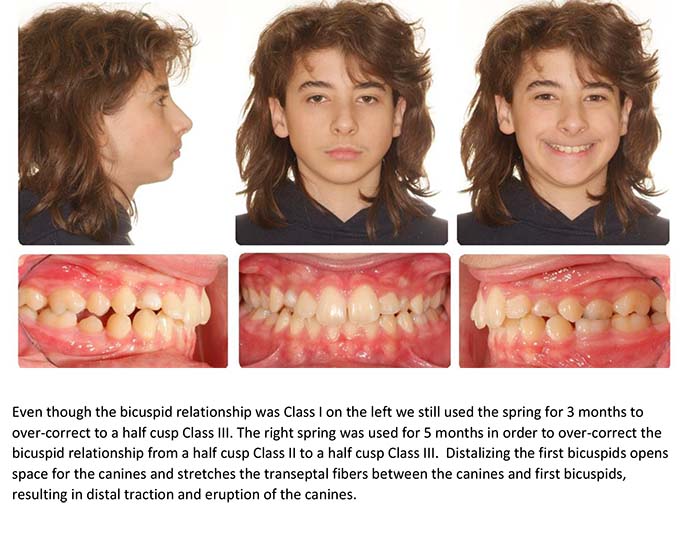
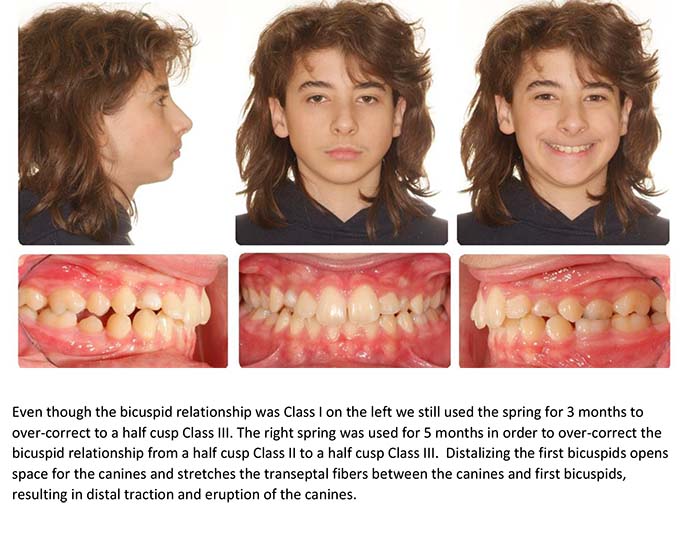
1. Xbow 2 months left spring, 3 months right spring 2. Compensatory maxillary expansion 3. Full braces

Sharing the correction between the upper and lower arches preserves upper lip fullness in patients with retrognathic mandibles
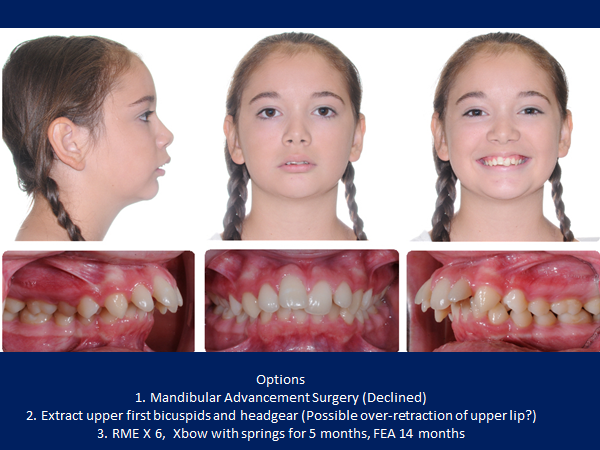

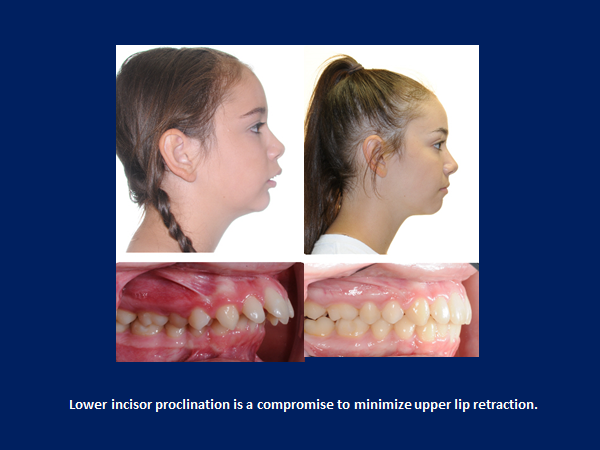
This case shows the importance of non-extraction treatment and not over-retracting the upper lip in a Class II patient with a convex profile.

Before

1. RMEX4 followed by Xbow, springs for 3 months. 2. Full braces for 1 year



Profile change after 7 months Xbow, after photo taken 2 months after spring removal
Initial to Progress after 7.5 months Xbow and maxillary expansion. Profile change possible with short lower facial height.
This case is an example of non-extraction treatment in a Class II crowded deep overbite malocclusion with a convex profile.

Initial
Progress after Xbow®, maxillary expansion, and upper canine alignment

Initial to Progress after 2X4 followed by 4 months Xbow followed by maxillary expansion



Progress after canine alignment to Progress after 6 months full braces



Initial to Progress after 6 months full braces


10 months full braces


2 years post deband



Initial to Progress after 2X4 followed by 4 months Xbow followed by maxillary expansion



Progress after canine alignment to Progress after 6 months full braces



Initial to Progress after 6 months full braces
Surgical correction to preserve the upper lip. Initial to 15 months total treatment time including lower bicuspid extraction site space closure and lower jaw surgery by Dr. Bill McDonald.




Initial


After lower bicuspid extraction site space closure and lower jaw surgery by Dr. Bill McDonald. The upper second molars are unopposed and can be removed if they ever cause a problem which is very rare.
There are only two upper molars in occlusion and the molar relationship is Class III. In these cases we look for a Class I bicuspid relationship. When a patient chooses surgery we concentrate on ideal facial esthetics.
The upper incisors are slightly proclined which prevents the upper lip from hanging straight down. This creates complementary curves between the nose and upper lip, and the lower lip and chin. Upper lip projection should be slightly ahead of the lower lip. Lower lip projection should line up with chin. The nose blends in beautifully with the face.
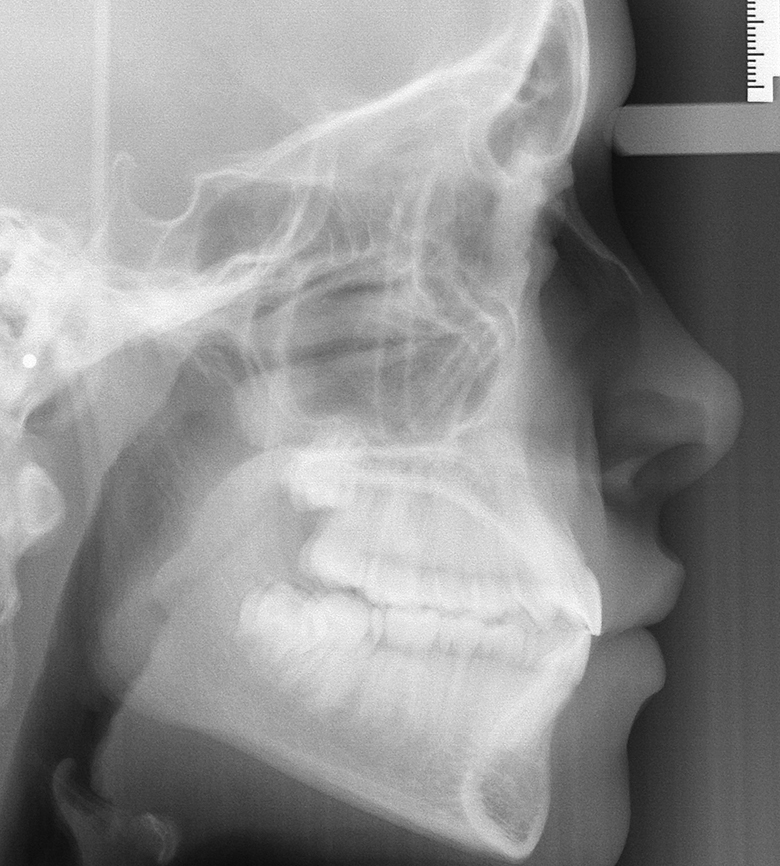
Below are pretreatment cephs with Class I skeletal patterns with good lip fullness, but different soft tissue convexity angles and midface development.
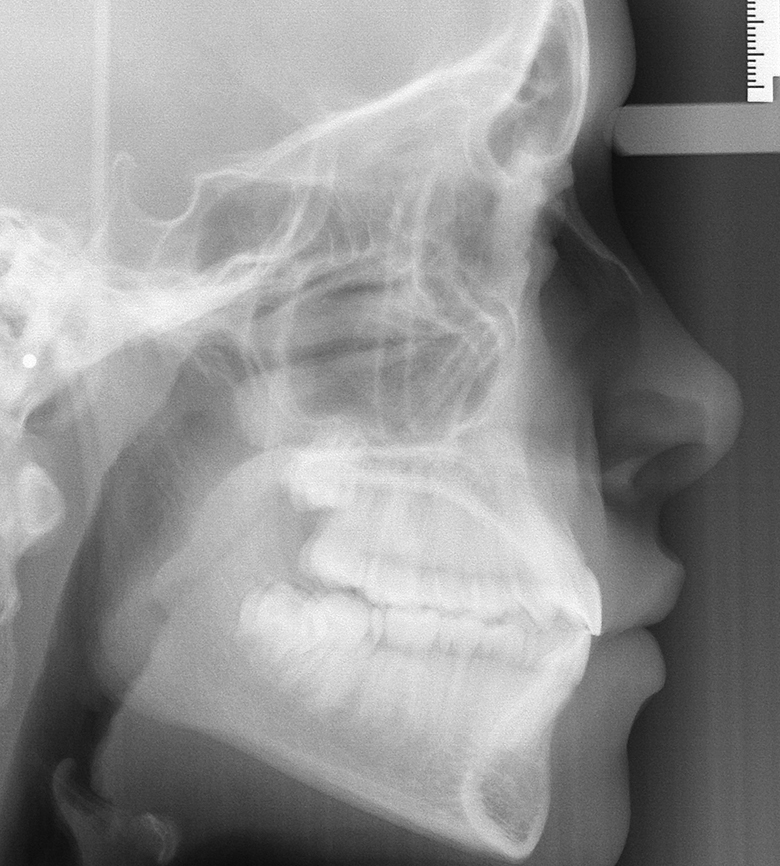
Patient #1 pretreatment ceph


Patient #2 pretreatment ceph
Patient #1: Class I skeletal, upper and lower incisors are naturally more proclined than established "norms". Lips are slightly protrusive and balanced perfectly to Rickett's E plane due to short nasal projection. Is a slight protrusion the new ideal?
Patient #2: Class I skeletal, high soft tissue convexity angle due to strong nasal growth , upper lip retrusive to Rickett's E plane.
The goal should be to maintain the upper incisor position. If this is not possible it is better to end up with a slight protrusion and long-term retention instead of a retrusion based on the wishful thinking of better stability. We cannot predict how much more nasal growth will occur, only that it will.
More Compromises
This is a common conversation I have with orthodontists that criticize Crossbow. It starts by an orthodontist saying he uses headgear to prevent lower incisor proclination. I ask what if the patient doesn't wear the headgear? The orthodontist will reply that they will add Class II elastics. I add that will procline lower incisors. They reply that they use a full size wire and -6 degree lower incisor brackets to prevent the lower arch from coming forward. (Myth) I ask what if the patient doesn't wear the elastics. They reply that is when they place Forsus Springs. I add that will push the lower arch forward. They reply not if they use a full size wire and -6 degree lower incisor brackets. (Myth)
I ask what if they see side effects like posterior openbite, upper molar flaring, or occlusal plane canting. They reply they add vertical elastics. I thought they wouldn't wear elastics. They reply the result will be a compromise:)
Lower incisor proclination is not ideal, but neither is orthodontic compensation when the ideal treatment is jaw surgery. Sometimes we get lucky and the patient and parents agree to ideal treatment. Sometimes we compromise.
The Debate Over Lower Incisor Proclination and Gingival Recession
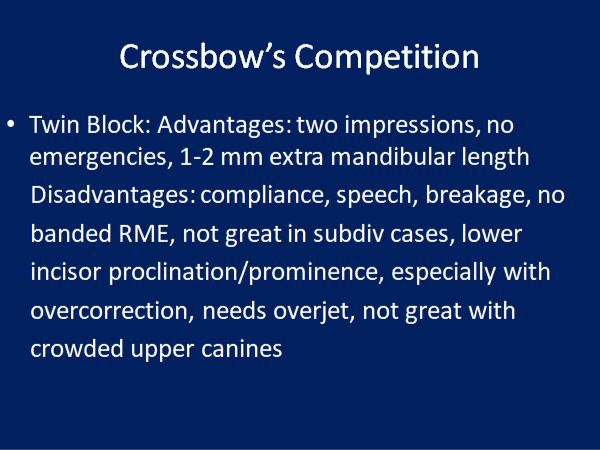
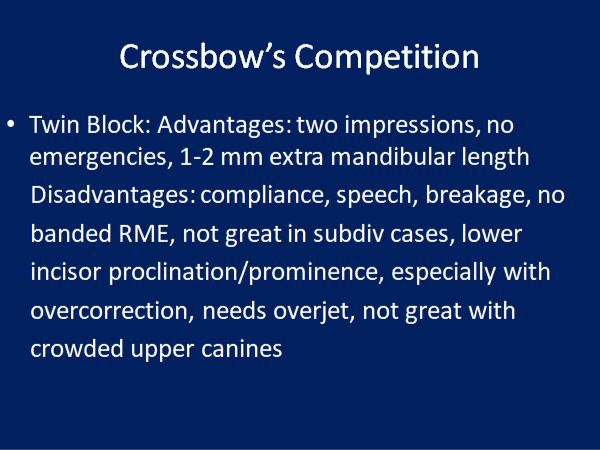
Crossbow’s Competition: Dealing With Side Effects
The Debate Over Lower Incisor Proclination and Gingival Recession
Part 1: Introduction
When I was an orthodontic resident in 1979 we were taught to treat an upright lower incisor. The only expansion allowed was a sutural expansion with an RME.
The "shared belief" was that lower incisor proclination would result in gingival recession.
In the 1980s my Class II patients fell into four groups.
- Orthodontic decompensation and jaw surgery,
- Two-phase non-extraction beginning with a functional appliance (which evolved into Herbst followed by Xbow),
- One phase four bicuspid extraction and headgear,
- One phase upper bicuspid extraction.
One thing became clear. If I extracted four bicuspids in a deep overbite case, I ended up chasing the lower incisors in what I call the "never-ending overjet". It was in these cases where I saw the most lip retraction or profile flattening.
I began treating more and more of these cases non-extraction and in two phases.
No matter which interarch Class II appliance I used, I proclined lower incisors. Whether it was Xbow or Herbst or Twin Block or Class II elastics or Forsus, it didn't matter. Expand buccally? Interproximal reduction?
Fill the slot and tie back? Minus six degree lower incisor brackets? They still proclined.
I didn’t worry about proclining lower incisors with functional appliances until I began using Herbst.
(So this is what happens with full-time wear.) Even then, I didn’t see any gingival recession which agrees with the article by Hans Pancherz and a systematic review on proclination. I am more comfortable with lower incisor tipping followed by partial uprighting with Xbow and non-edgewise Herbst than I am with bodily mesialization with a rectangular archwire and minus six degrees lower incisor brackets, which I find results in root prominence.
Dr. Anthony Mair explains it this way: "It is better to tip the crown and leave the root in bone than to bodily move the root out of bone; this setup is more reflective of natural compensation."
Dr. Mair has recently reported on several cases where Class II elastics used against a lower aligner caused bony dehiscence due to bodily movement of the lower incisors. The solution was to torque the root apex back into alveolar bone as recommended by Dr. Laursen et al (Am J Orthod Dentofacial Orthop 2020;157:29-34)
Dr. Mair warned that we should prepare for more of these cases as the popularity of Class II elastics used with aligners increases.
Part 2: The history involving my 40 years as an orthodontist
1979-1981: I was an orthodontic resident at Indiana University. Class II's were treated by bicuspid extraction and headgear. Class II elastics were discouraged. We heard Drs. Rocke and Kesling speak on treating non-extraction with Class II elastics. They showed ceph tracings similar to what other orthodontists were achieving with functional appliances such as activators, bionators, and Frankel appliances. It was a combination of skeletal and dental effects including lower incisor proclination.
Dr. Ricketts was making an impact on our profession when he introduced the soft tissue analysis and the "Esthetic Plane". He said that over-extracting could be detrimental to the face. He suggested that lower crowding in a deep bite was related to the lower arch being contained by a constricted upper arch.
The lower incisor tends to be more proclined in low mandibular plane angle cases with a normal overbite and more upright in high mandibular plane angle cases with a normal overbite. Dr. Ricketts taught that four bicuspid extractions should be done more in high angle cases with a shallow overbite. Low angle cases with deep overbite should be treated non-extraction.
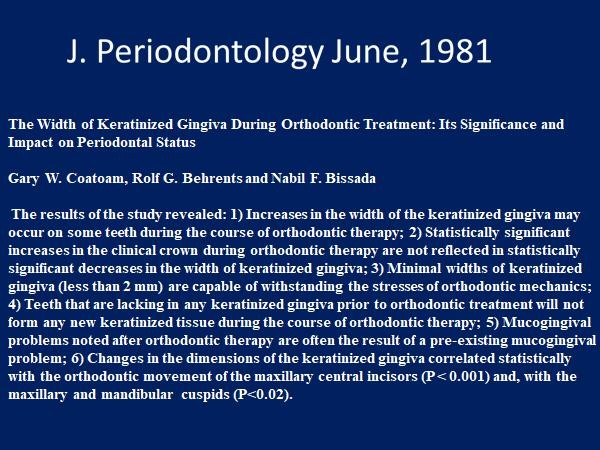
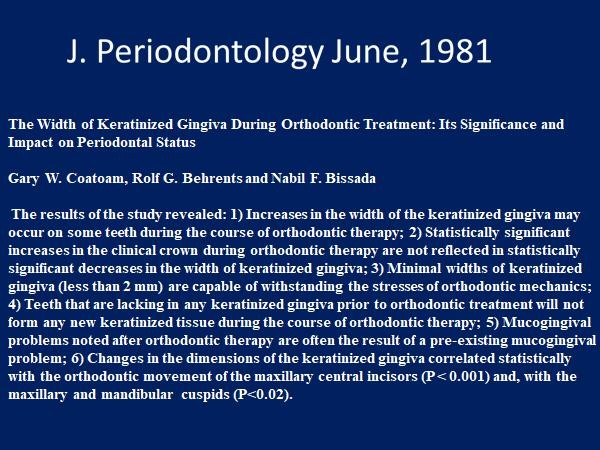
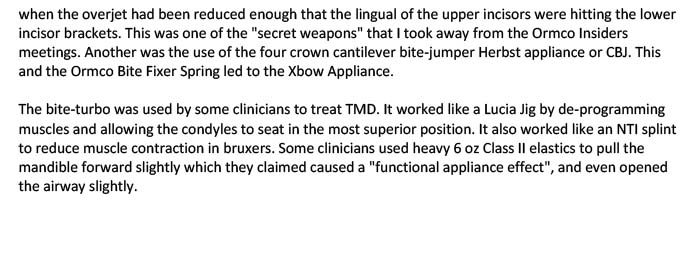
1981: Dr. Behrents published the groundbreaking article in the Journal of Periodontology that was the first to debunk myths that I had been taught.
1981-1984: I was an associate with my mentor, Dr. Michael Wainwright. He taught me indirect bonding, two-phase treatment, and combined orthodontic/orthognathic surgical treatment.
1984: I opened my office in North Delta. I began using functional appliances. I took a ceph at the final records.
I was proclining lower incisors with the functional appliances, but I was not seeing gingival recession. This became a subject that would interest me for my entire career.
Dr. Casko published his findings that questioned Tweed's 95-degree IMPA in untreated Class II skeletal patterns with Class I occlusions. More myth debunking.
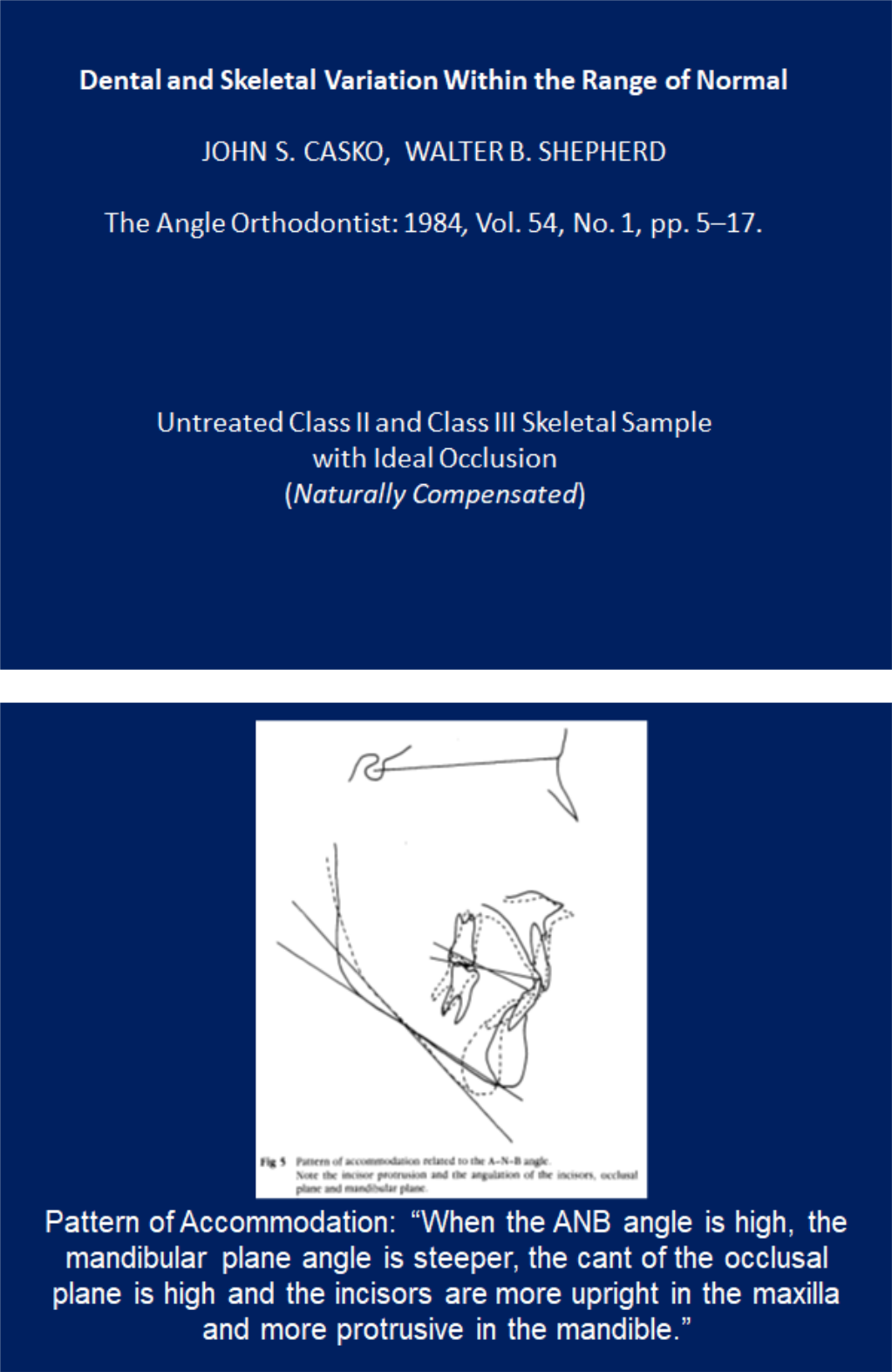
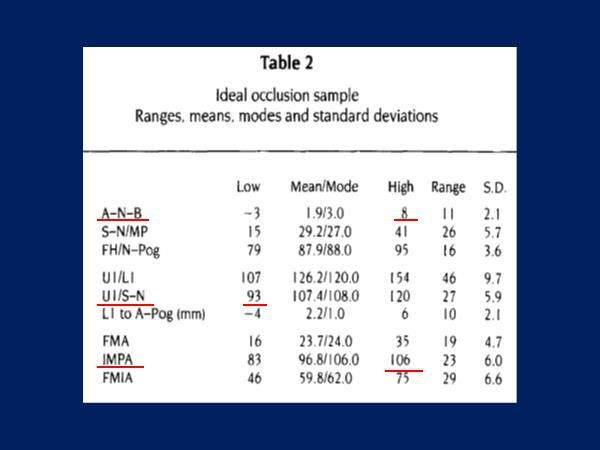
Dr. Casko believed that incisor inclination was linked to the skeletal pattern and showed that it was normal for the lower incisor to have an IMPA higher than 95 degrees in an untreated skeletal Class II with a Class I occlusion.
He argued that this should be the goal for Class II compensation.
Example from my practice:


Naturally occurring Class II skeletal with Class I dental and a retroclined upper incisor and proclined lower incisor
Dr. Creekmore agreed with Dr. Casko.
1990: My study club invited Dr. William Clark to speak to us about twin blocks. I began using them.
1991: Dr. DeVincenzo publishes his research which is the first of many to question the ability of functional appliances to increase mandibular length in the long term. Dr. Lysle Johnston coined the term "mortgaging mandibular growth".
More myth debunking.
1995: I began using the four crown Herbst appliance which got me interested in non-compliance appliances.
My main concern was with over-correction I was seeing noticeable lower incisor proclination that I had not noticed with removable functional appliances. I tried placing -5 to -10 degree lower incisor brackets but instead of proclining the lower incisors I noticed that the bodily mesialization of the incisors resulted in a "washboard effect". I preferred tipping the lower incisors temporarily and then allowing them to upright before phase two.
The important thing was I did not see the gingival recession that I had been taught would happen.
Dr. Alan Lowe developed the Klearway appliance for snoring and sleep apnea. Long term wear has resulted in severe proclination of lower incisors without significant recession.
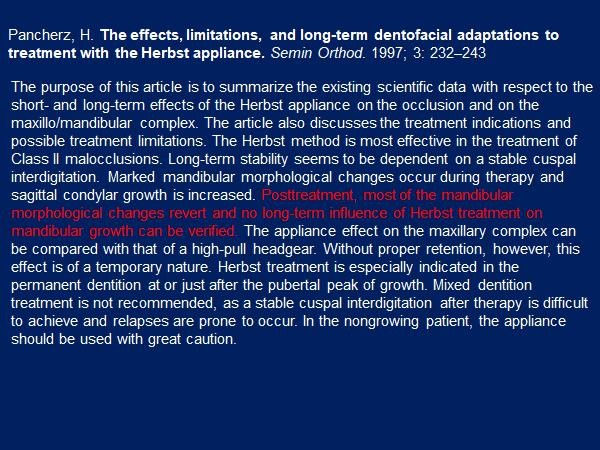
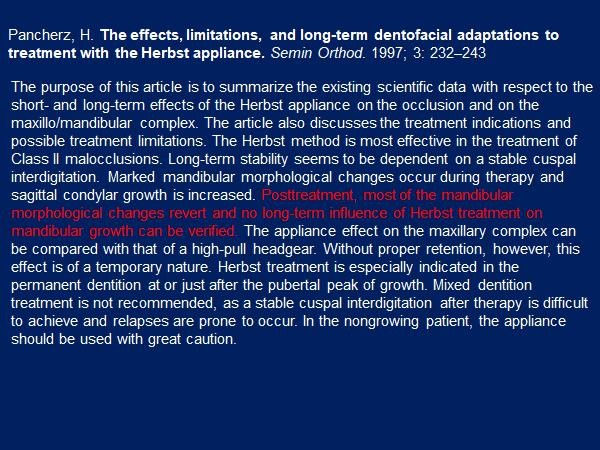
1997: Dr. Pancherz published his summary of the effects of the Herbst appliance. There was no long term increase in mandibular length. He did not recommend it in non-growing patients, possibly due to the risk of condylar resorption, which he had shown. (Dr. Woodside also showed condylar resorption with the Herbst appliance. When I lectured at the University of Toronto, Dr. Woodside commented that the Crossbow Appliance was probably kinder to the condyle than the Herbst appliance because the springs were stress breakers and allowed the condyle to function in the fossa.)
The takeaway message was that mixed dentition treatment was not recommended because "a stable cuspal interdigitation after therapy is difficult to achieve and relapses are prone to occur." Pancherz had proven what Dr. Herbst called "the bite catching effect".
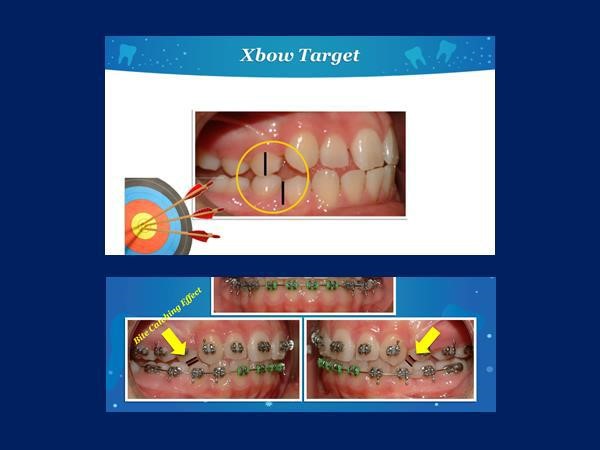
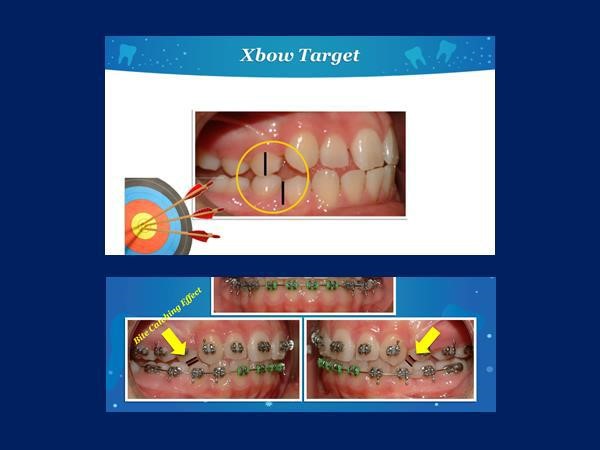
Thanks to Dr. Herb Hughes for the above slide showing over-correction with Xbow and the bite catching effect of the steep cuspal inclines of the first bicuspids.
1998: Dr. Jay Bowman published an article in the JCO using Jasper Jumpers attached to a lower lip bumper instead of a bypass. I was convinced that most Class II's required maxillary expansion. I was also using lower lingual arches to preserve the "e" space. I added a lip bumper and Ormco's Bite Fixer springs. This led to the Xbow appliance.
Dr. Pancherz publishes his findings on the Herbst appliance and gingival recession.
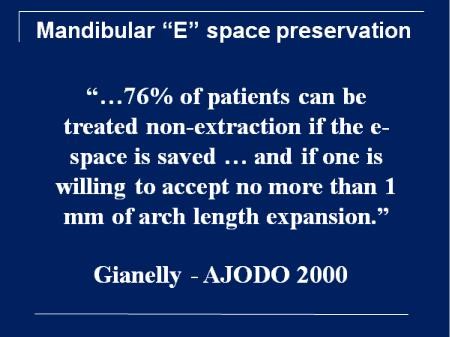
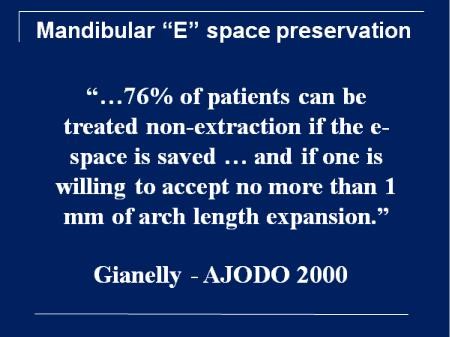
2000: Dr. Gianelly gives us a target to shoot for.
2001: Granted a US patent and registered trademarks for the Xbow
2002: I lectured on the Xbow appliance with Dr. Pancherz at the GLAO/MASO meeting. We discussed lower incisor proclination and agreed that temporary over-proclination followed by uprighting did not cause a gingival recession and in fact over-correction followed by the bite catching effect and cuspal interdigitation was necessary for long term stability.
2009: First Xbow research paper published in the AJODO after working with Dr. Carlos Flores-Mir at the U of Alberta.
We showed the lower incisor proclined a similar amount to the Herbst appliance. A total of seven papers on Xbow would be published as a result of Dr. Flores-Mir's effort.
2013: Drs. Bob Miller and Carlos Flores-Mir publish the definitive research paper on the efficiency of two phase Xbow treatment compared to one phase Forsus to the arch wire treatment.


2015: The data from 172 consecutively treated Xbow patients was studied at the U of Alberta. An interesting finding was that the average initial lower incisor inclination was 99 degrees. This agrees with Dr. Casko's belief that Class II skeletal cases are naturally compensated.
2016: I was asked to speak at the AAO Scientific Session. My conclusion was that the results are similar for all inter-arch Class II appliances. The differences are probably not clinically significant. We should be focusing on preserving the upper lip and treatment efficiency, including decreasing the treatment time in full edgewise appliances.
2017: Dr. Gianelly's 76% non-extraction target looks right on.
The eye-opener:
2019:
These are some heavy hitters in our profession. Dr. Buschang's research has shown there is little evidence to prove that lower incisor proclination causes gingival recession. Dr. Behrents told us in 1981 that some recession was normal and that severe recession could be prevented as long as there was an attached gingiva present or a graft placed before ortho.
Dr. Lindauer asked me to speak on Crossbow at the AAO in 2016.
Part 3: Ancient History
Dr. Angle's Class II "bite-jumping" appliance, photo courtesy of Dr. Lysle Johnston. This would have resulted in lower incisor proclination. If this caused gingival recession Dr. Angle would have reported it.
Dr. Angle's students, Begg and Tweed, stopped doing what they had been taught and followed the teachings of Calvin Case. Dr. Tweed was able to control the torque of the upper incisors as he retracted them to reduce the overjet in Class II's. He was also able to level the Curve of Spee with full-size rectangular archwires and Class II elastics to erupt the lower posterior teeth. When you just looked at the model's Tweed was able to make a Class II case look like an ideal Class I skeletal-dental, complete with upright incisors. In 1930 Dr. Broadbent invented the cephalometer, which allowed Tweed to measure the inclination of the incisors and compare his results to untreated Class I dental-skeletal patients. This led to the Tweed Triangle and the goal of treating an upright lower incisor. Tweed was known for saying, "Put your plaster on the table," but it was the cephalometric measurements that gave scientific support to the upright lower incisor.
It wasn't until 1956 that Tweeds results were studied closely by Drs. Stoner and Lindquist at Indiana University. Their study "Consecutive Cases Treated by Dr. Charles Tweed" was published in the Angle Orthodontist.
It looked at the claim that Tweed mechanics resulted in improved facial esthetics.
The main finding was that overjet reduction was almost all by upper incisor retraction.
I met Dr. Lindquist while I attended Indiana University. He was the first orthodontist that I heard warn of over-extracting. He said that serial extracting was a "self-fulfilling prophecy" in that extracting primary canines increased the odds that first bicuspids would need to be extracted. He advised to only extract lower primary canines if the lateral incisors were impacted or blocked out.
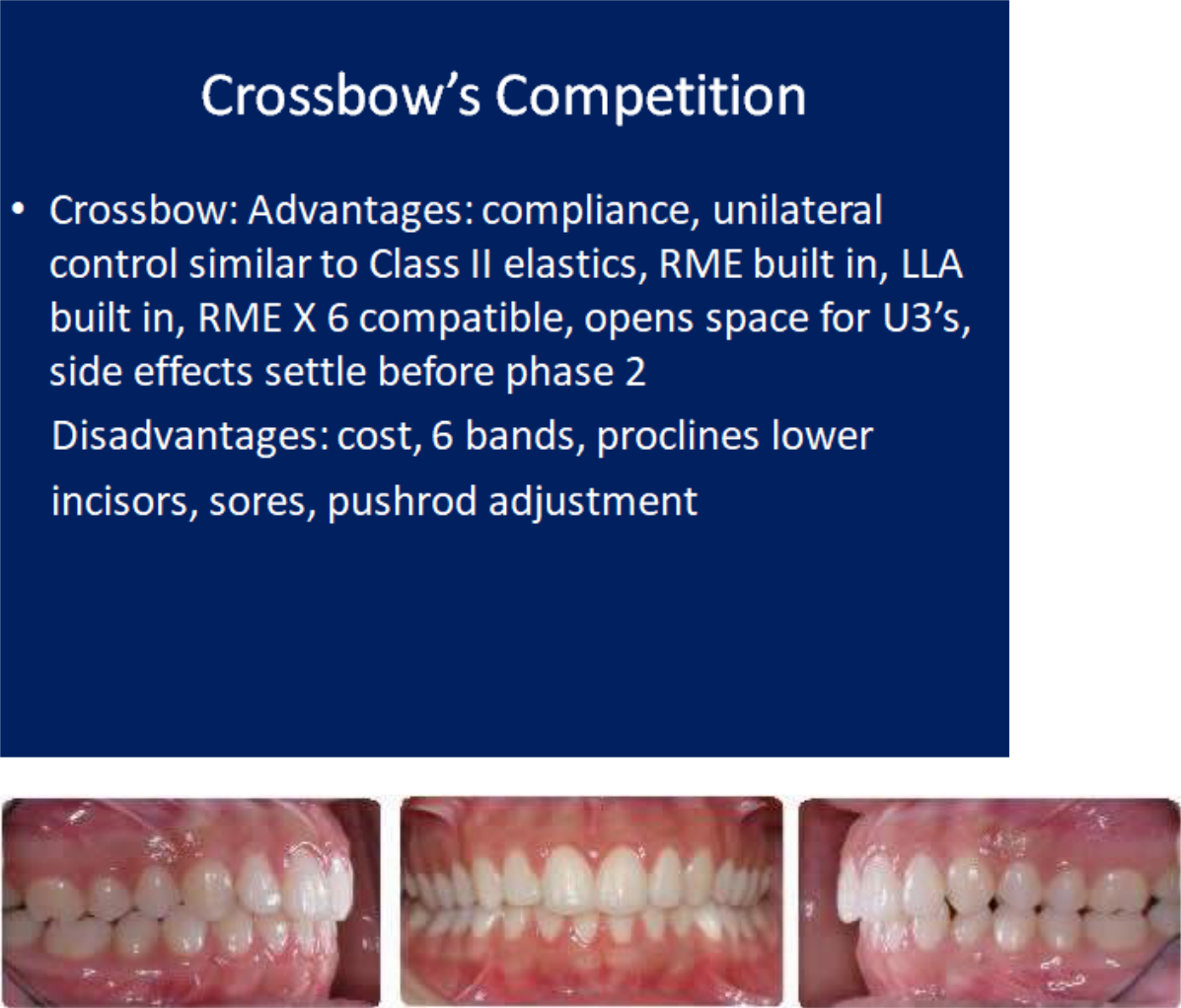
Crossbow's Competition and Dealing With Side Effects


Bite opening in phase two with eruption mechanics (bite turbo and Class II elastics) while the patient is growing and mandibular growth can compensate for the downward and backward rotation of the mandible.
Initial unilateral Class II


Left spring only


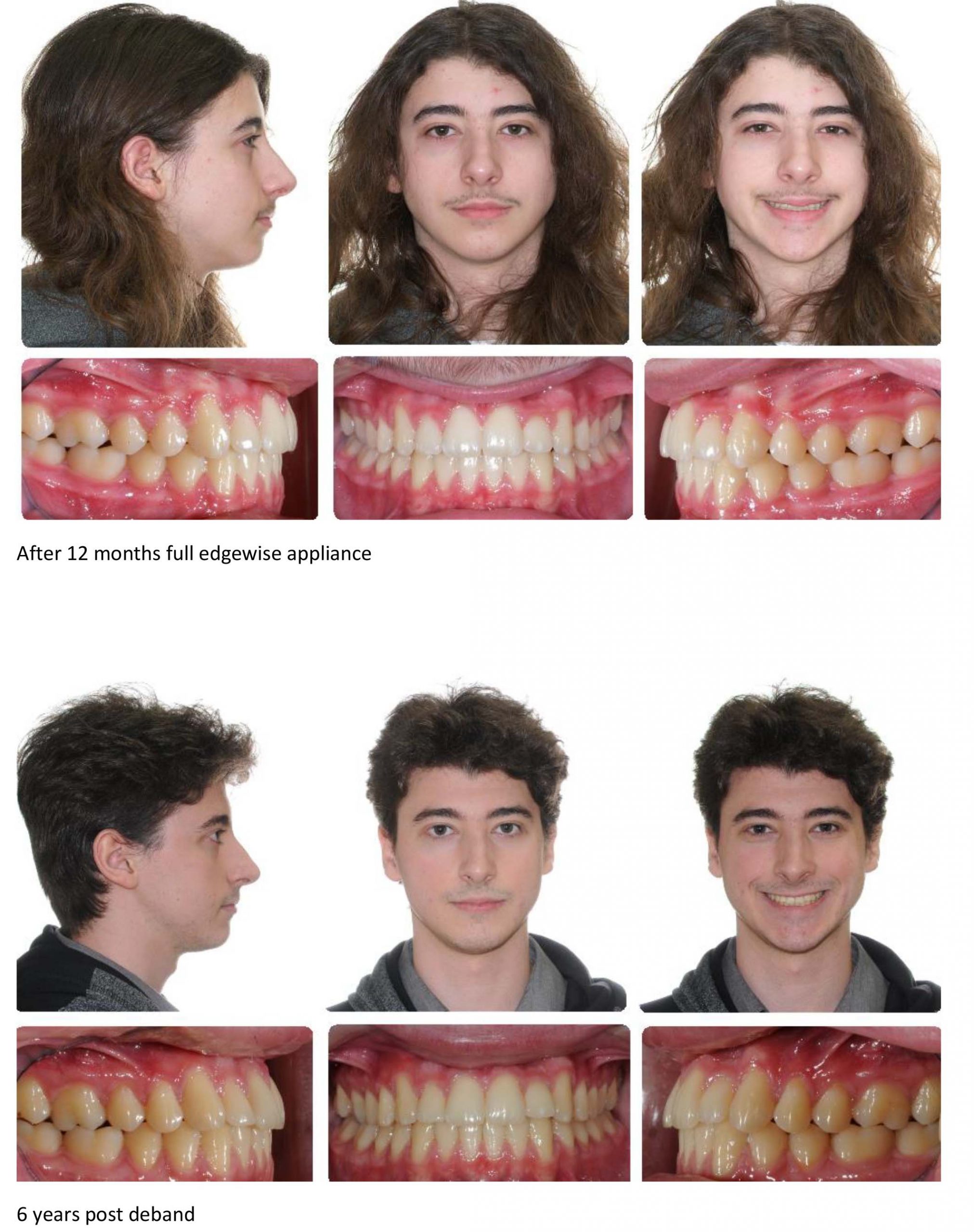
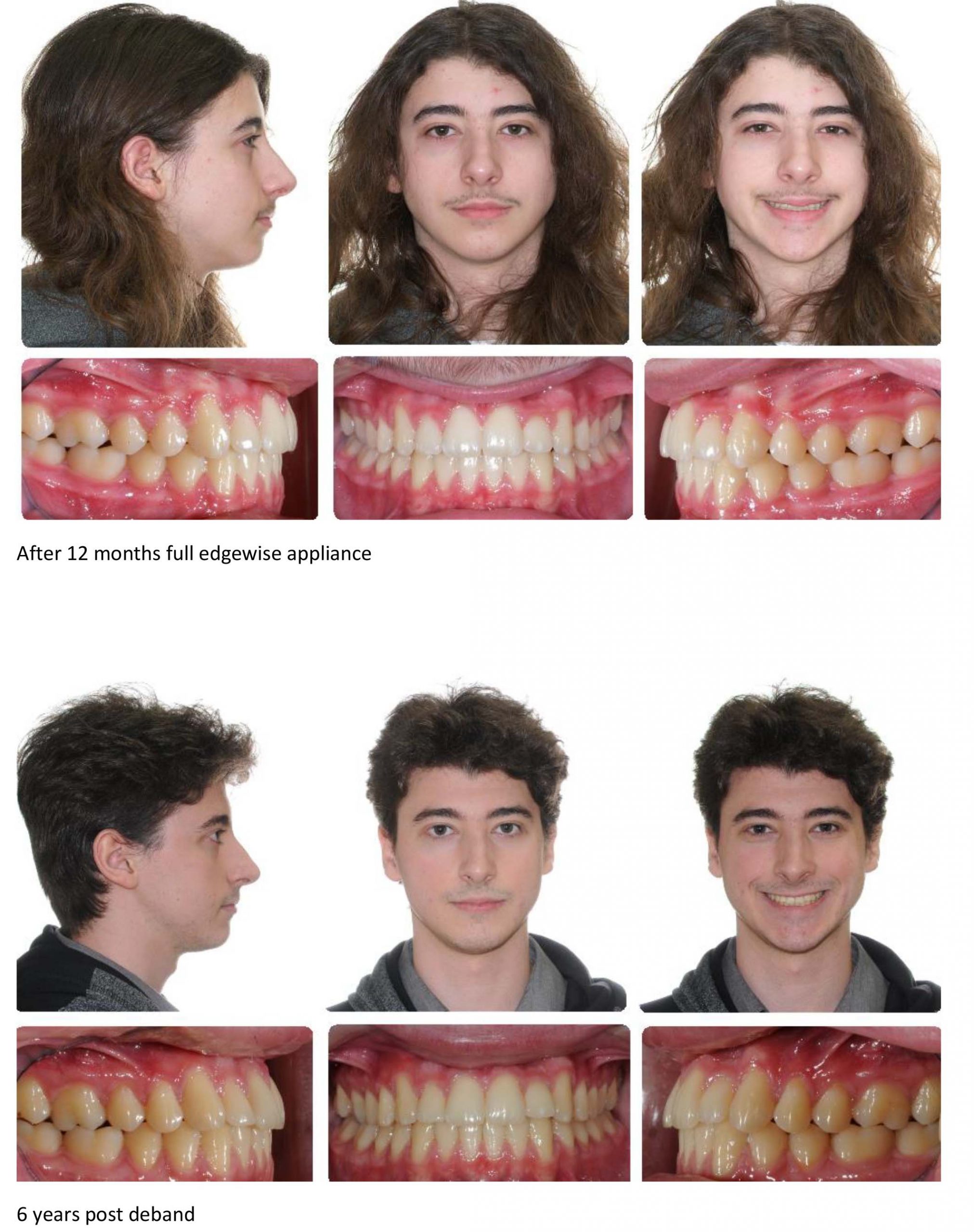
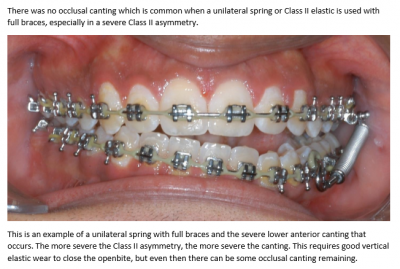
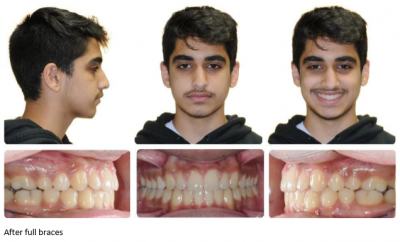
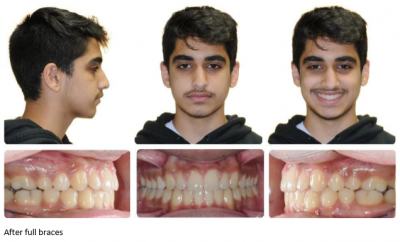
Over-correction after 5 months, incisors edge to edge, note side effect of posterior openbite but no anterior occlusal canting


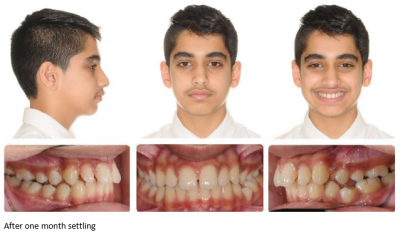
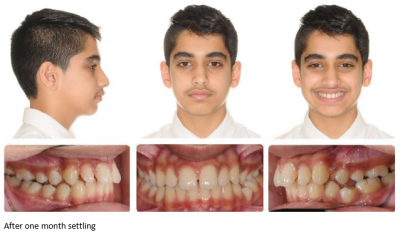
After 1 month settling


After 2 months settling


After 5 months settling


This is an example of why we segment the arch wire distal to the canine before placing springs.


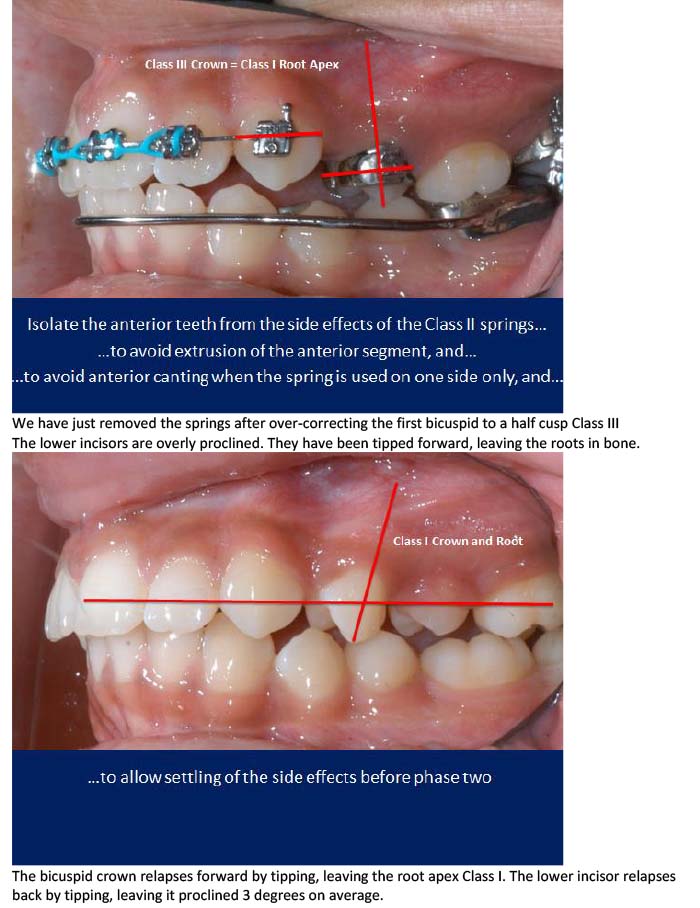
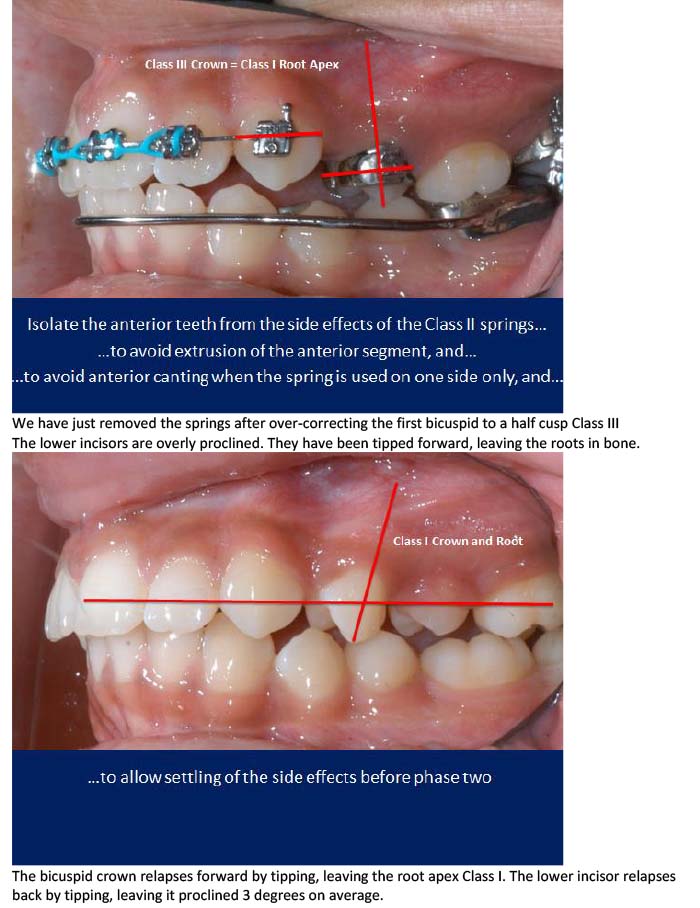
We have just removed the springs after over-correcting the first bicuspid to a half cusp Class III
The lower incisors are overly proclined. They have been tipped forward, leaving the roots in bone.
The bicuspid crown relapses forward by tipping, leaving the root apex Class I. The lower incisor relapses back by tipping, leaving it proclined 3 degrees on average.
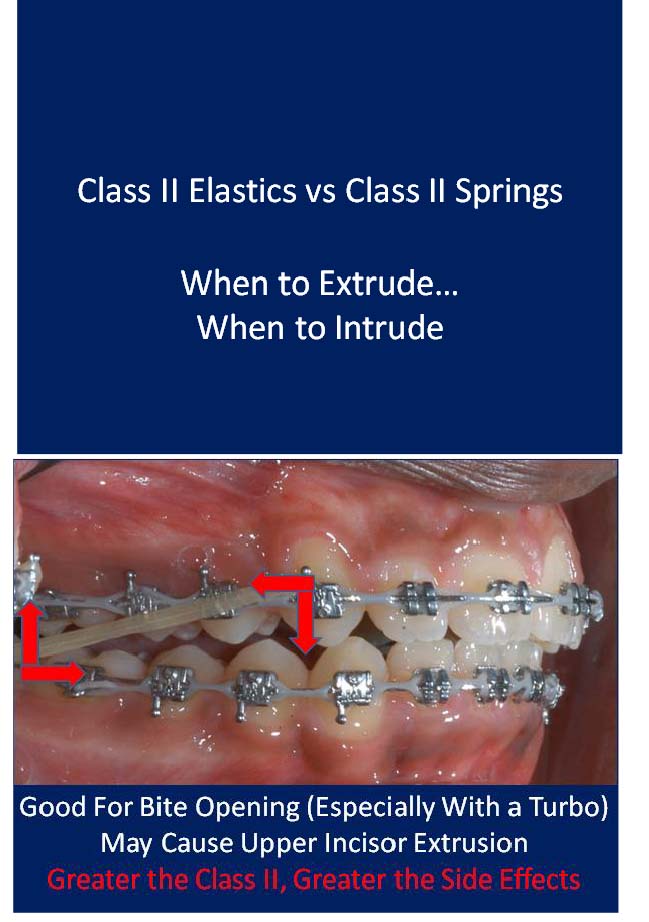
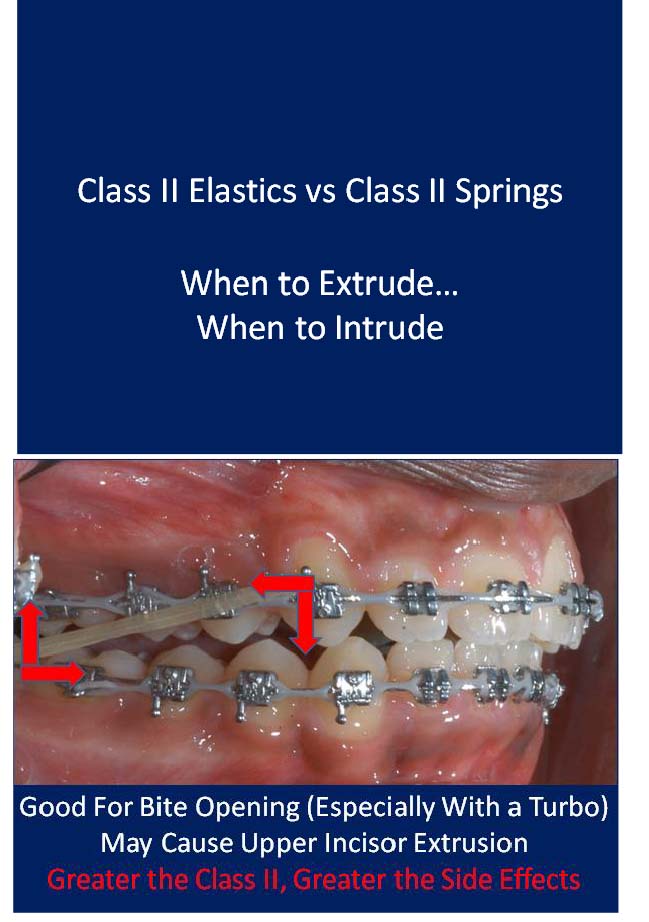
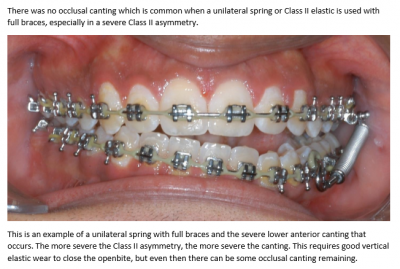
The greater the Class II, the greater the side effects from Class II elastics and Class II springs.
Class II elastics cause tooth eruption, which does not tend to relapse. Class II springs cause tooth intrusion and posterior open bite which does tend to relapse. Over-eruption of upper incisors (and upper canines with phase one Class II elastics) can lead to a gummy smile.
A unilateral Class II elastic on a full edgewise appliance (FEA) is no problem.
A unilateral phase one Class II elastic is likely to cause an occlusal cant that might be unrecoverable.
A unilateral Class II spring on an FEA can also cause an occlusal cant and an open bite that requires good anterior vertical elastic cooperation to resolve. A unilateral spring on an Xbow does not cause a cant because there are no brackets on the lower incisors. Any unilateral intrusion will relapse.
Class II springs with an FEA cause buccal flaring of upper molars, which may require posterior crossbite elastics to recover from. Class II springs on an Xbow do not cause the same flaring because of cross arch stabilization by the RME.
Both Class II elastics and Class II springs cause proclination of the lower incisors. Dr. Anthony Mair has warned about the use of Class II elastics with lower aligners, which cause bodily root movement, root prominence, and gingival recession of the lower incisors.
Xbow causes a temporary over-proclination of the lower incisors followed by partial but incomplete uprighting.
This is necessary in order to over-correct the Class II buccal relationship and to achieve the "bite-catching effect," and a socked in Class I bicuspid relationship BILATERALLY!
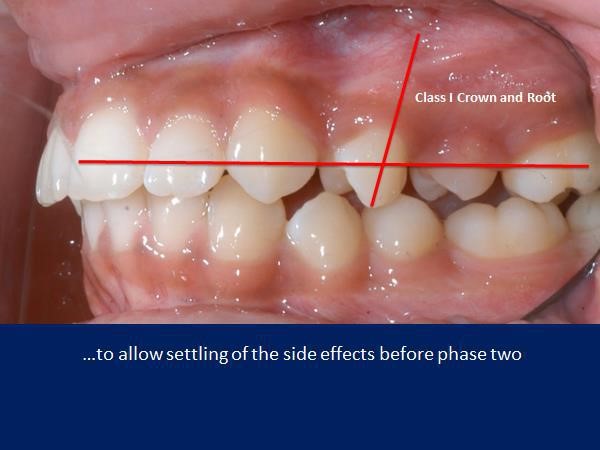
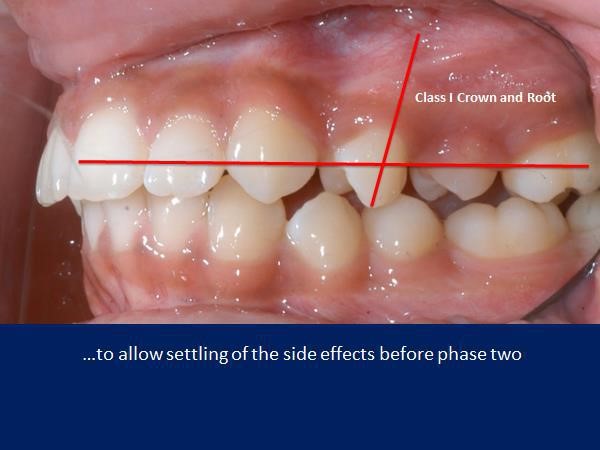
The fact that the Xbow is a phase one appliance allows the clinician to achieve RAPID over-correction of the sagittal and transverse problems soon after the eruption of the first bicuspids to take advantage of the "bite-catching effect" of the steep cusps of the first bicuspids. The side effects such as posterior open bite and over-proclination of the lower incisors tend to relapse before phase two full edgewise.
The clinician has a better idea of where the incisors will end up after phase two and can modify the treatment plan at the beginning of phase two.
If there is still a deep overbite to treat in phase two, then a combination of a bite-turbo and Class II elastics maybe use for rapid bite-opening. The patient only has to cooperate with elastics for a short time so burnout is not as big a problem compared to depending on Class II elastic use in phase one and phase two to correct the entire malocclusion. There is also less chance of over-erupting the upper incisors with short term use of the Class II elastics.
Longer treatment time with Forsus to the archwire is due to dealing with the spring side effects late in treatment, such as posterior open bite and buccal flaring of the upper molars. The greater the correction, the greater the side effects, and the longer it takes to deal with them.
There is no buccal flaring of the upper molars with Xbow.
Much of the posterior open bite and proclination of the lower incisors rebound before full braces are placed.
Drs. Miller, Tieu, and Flores-Mir's article titled "Incisor inclination changes produced by two compliance-free Class II correction protocols for the treatment of mild to moderate Class II malocclusions" is in the online version of the Angle Orthodontist.
It is based on Dr. Bob Miller's clinical study.
He compared 36 Class II patients treated in one phase with Forsus to the archwire in a full edgewise appliance to 38 similar Class II patients treated in two phases with Xbow followed by a full edgewise appliance. The Forsus to the archwire group was finished in an average of 30.2 months (between records). The Xbow group was finished in an average of 24.2 months (between records), which included a 4 to 6 month rest period to allow for relapse. The two-phase Xbow patients were completed 6 months faster on average than the one phase Forsus to the archwire patients (time between records).
The Forsus to the archwire group had full braces for an average of 26.75 months. The Xbow group had full braces for an average of 16.68 months or 10 fewer months. There was no significant difference in the lower incisor to the mandibular plane angle between the two groups. The Xbow patients ended up with lower incisors at an average of 100 degrees to the mandibular plane, which is considered a reasonable compromise for non-extraction Class II compensation.
Editor's note: Longer treatment time with Forsus to the archwire is due to dealing with the spring side effects late in treatment, such as posterior open bite and buccal flaring of the upper molars. The greater the correction, the greater the side effects, and the longer it takes to deal with them. There is no buccal flaring of the upper molars with Xbow.
Much of the posterior open bite and proclination of the lower incisors rebound before full braces are placed.


The side-effects of Forsus on the archwire are especially problematic when the spring is used unilaterally late in treatment.
The unilateral posterior openbite and anterior canting requires prolonged treatment with good elasitc cooperation to recover.
We do not see the anterior canting when the spring is used unilaterally on a Xbow because there are no lower brackets.
The fact that the first bicuspids are already Class I after Xbow therapy reduces the time in phase two braces and the need for side-effect correction with elastics.
I use the same principles when using the Forsus device with a full edgewise appliance as I do with Xbow.
Use the 22mm Direct Pushrod distal to the lower first bicuspid instead of the canine, if possible.
This keeps the Forsus device more compact and moves it distal to the anterior curvature of the arch, preventing the need for rod adjustments. It also keeps the spring distal to the Obicularis Oris muscle, preventing sores.
The only difference is you cannot fully compress the spring with an edgewise appliance if you use a bracket as the anterior stop.
If you do be prepared to rebond the bracket. Don't forget to steel tie the first bicuspids.
Reactivate the springs with crimpable stops on the rods or use longer rods. Dr. Bob Miller taught us to hook up the pushrod using an Alastic KX module to activate the spring but at the same time remove the force from the canine or first bicuspid bracket. This also negates the need to cinch the distal end of the arch wire.
Place the springs and pushrods as you would normally but don't close the loop yet. Make the pushrod adjustments leaving 1mm of play in the spring, remove the pushrod, pre-stretch a KX-1 module, place the KX module on the pushrod, place the pushrod on the archwire, close the pushrod loop, hook the KX module to the first molar hook using floss and a floss threader over the second bicuspid bracket and down between the second bicuspid and first molar, then place the pushrod in the spring. This completely activates the spring without debonding the canine or first bicuspid bracket.
If we place the 22 mm or 25 mm pushrod distal to the first bicuspid we use a KX-1 module.
We also use a KX-1 module distal to the canine in a bicuspid extraction case.


Alastic KX-1 module placed with floss threader


Alastic KX-1 module and lingual tuck-in pushrod adjustment on 25mm rod


Alastic KX-1 module hook-up distal to canine (severe Class II, patient decided against mandibular advancement surgery after preparation)


Alastic KX-1 Module hook-up distal to first bicuspid


Alastic KX-1 Module hook-up distal to canine (bicuspid extraction) with a 22 mm pushrod.
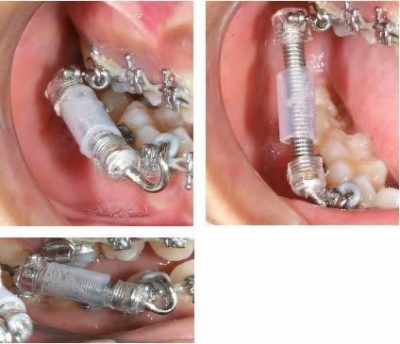
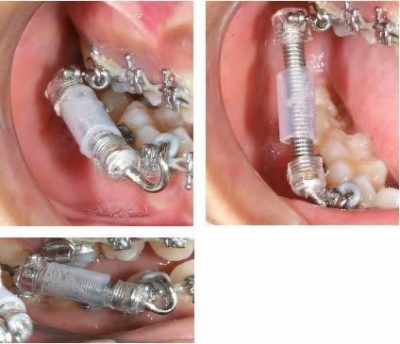
Spring Sleeve available from Comfort Solutions
Upper Airway Changes after Xbow appliance Therapy Evaluated with CBCT Angle Orthodontist, Vol 84, No 4, 2014
Conclusions
- Treatment with the Xbow appliance in Class II patients resulted in favorable dental and skeletal changes in the direction of a Class II correction.
- In cephalometric and three-dimensional evaluation of the upper airway, increase in the oropharyngeal airway dimensions and volume was observed.
There were no changes in the nasopharyngeal region and adenoid tissues.
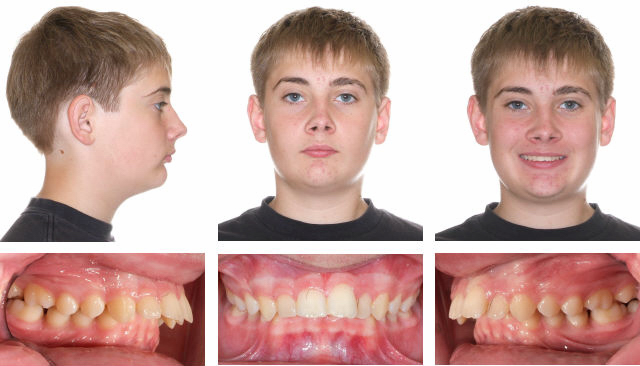
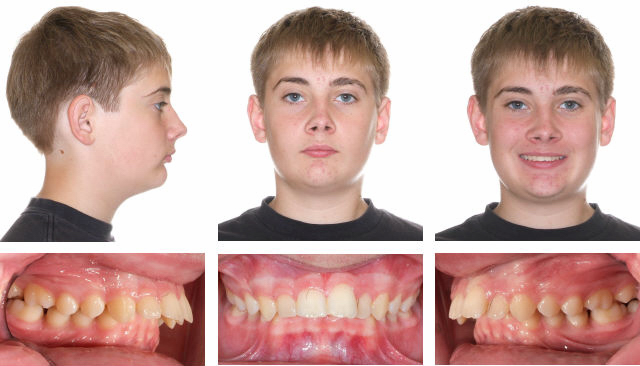
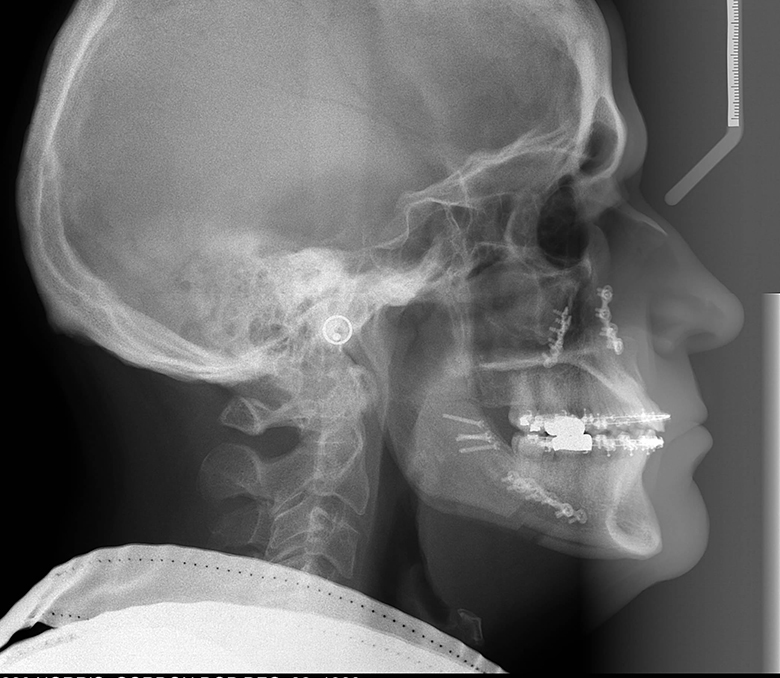
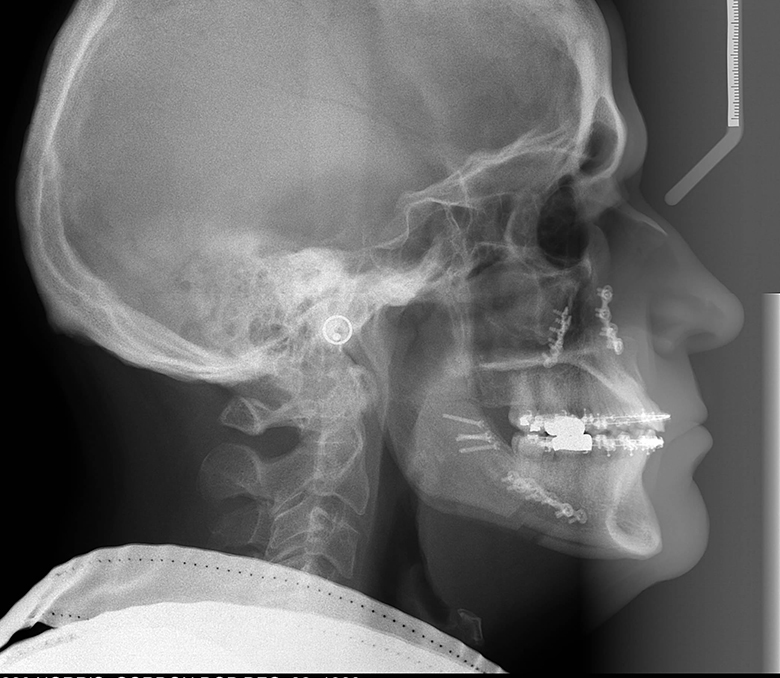
Before


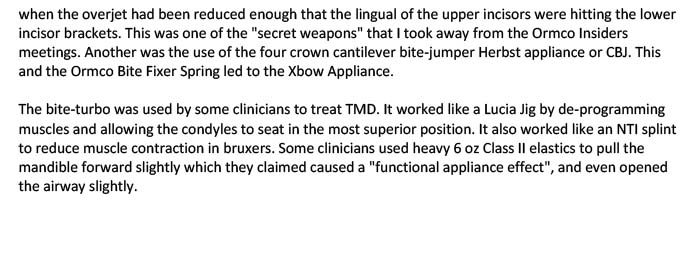
After 8 months Xbow, no expansion needed, after photos taken 1 month after springs removed, cephs below.


Positive airway change.


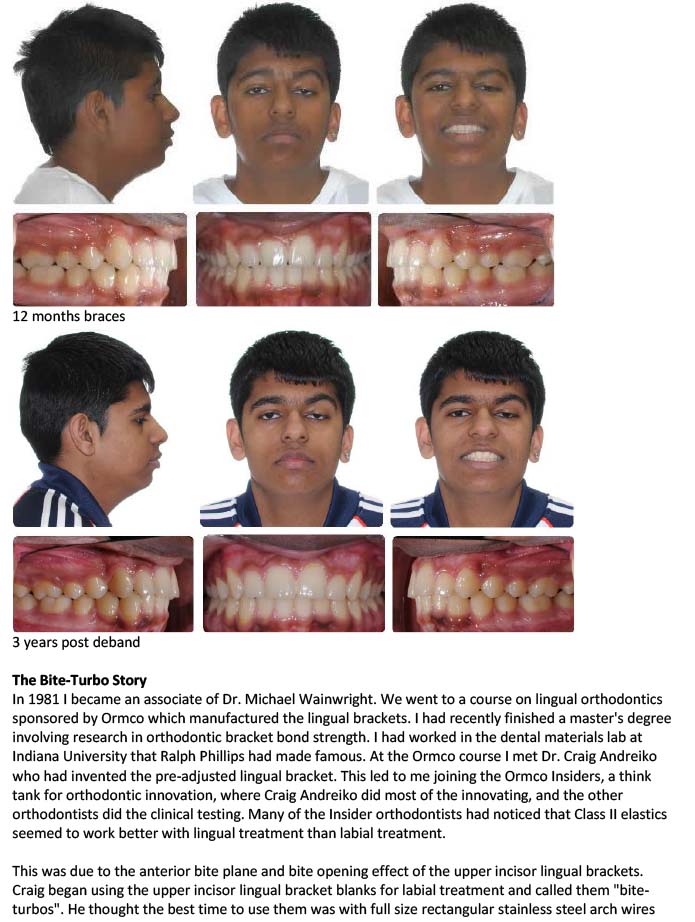
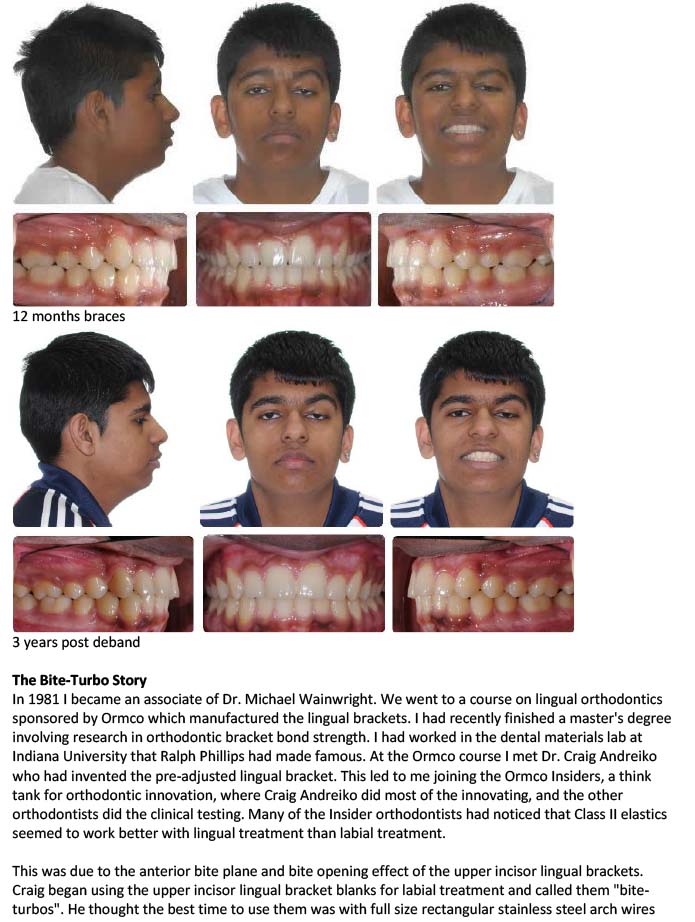
12 months braces.
Airway before and after maxillary and mandibular advancement surgery by Dr. Bill McDonald.
The patient was previously treated for sleep apnea with an intraoral mandibular repositioning appliance which gave temporary relief until the malocclusion which resulted from tooth movement became too great. She stopped the intraoral appliance and used a CPAP machine until the time of her surgery. She has not needed CPAP since her jaw surgery.


Superimposition of before and after surgery ceph tracing for above patient.


Initial for above patient.


After 14 months including two jaw advancement surgery.
Airway before and after maxillary and mandibular advancement surgery by Dr. Bill McDonald. The combined orthodontic/orthognathic surgery was done to treat a malocclusion, but the patient coincidentally had severe sleep apnea and was being treated with CPAP. The patient stopped using CPAP immediately after the surgery.


Dr. Reginald H.B. Goodday, associate professor and head, division of oral and maxillofacial surgery, Dalhousie University was on an expert panel with Dr. Higgins on the treatment of Class II malocclusion at the 2014 Canadian Association of Orthodontists Scientific Session. Dr. Goodday spoke on the orthodontist's and surgeon's role in the treatment of Obstructive Sleep Apnea.
He said "In patients with identifiable anatomic abnormalities of the maxilla and mandible resulting in a narrow pharyngeal airway, orthognathic surgery appears to be an excellent treatment option." In a recent communication the author asked Dr. Goodday to review the following section for accuracy. He added: "My intention was to provide information that would encourage this specialty to think long term when recommending treatment options to young patients. I also feel that patients should be informed of an underlying jaw deformity and why it should be considered when deciding on treatment options." His advice to orthodontists included the following:
- Severe Class II skeletal patients with retognathic mandibles may develop OSA.
- These patients are best treated with combined orthodontic/orthognathic surgery with mandibular advancement and possibly maxillary advancement as well.
- In these cases orthodontic decompensation gives the best esthetic and airway result. Decompensation involves non-extraction in the maxilla and two bicuspid extraction in the mandible.
- In young patients with Class II skeletal patterns that choose a non-surgical treatment plan, thought should be given to consevative treatment that will allow combined orthodontic/orthognathic surgical treatment to be done in the futrure.
Non-surgical treatment planning should keep in mind the following points:
- Pure upper incisor retraction in a severe mandibular retrognathic patient may result in an unesthetic increase in the naso-labial angle.
- This may lead to posterior positioning of the tongue.
- It also makes it difficult for the future surgeon to achieve an esthetic result as well as normalizing the airway. The maxilla may need to be advanced more than if the upper arch was previously treated non-extraction.
- Four bicuspid extraction to retract the incisors and close an anterior openbite may encroach on tongue space.
If the lower incisors are proclined and the profile is convex with a retrognathic mandible, the best treatment may be the extraction of lower first bicuspids, the retraction and uprighting of the lower incisors, and mandibular advancement surgery, with possible maxillary surgery with posterior impaction if a skeletal openbite exists.
- In severe cases where surgery is the only option and the patient declines but still wants some improvement, alignment only and leaving the malocclusion may be the best alternative, instead of over-retracting the upper incisors.
- Take a family history of snoring and sleep apnea.
- Consider early maxillary expansion and a non-extraction approach in borderline extraction patients instead of serial extractions.
- Refer for possible adenoid and tonsil removal in airway obstructed patients. If the maxilla is constricted a combination of maxillary expansion and adenoid and tonsil removal has been shown to give the greatest improvement.
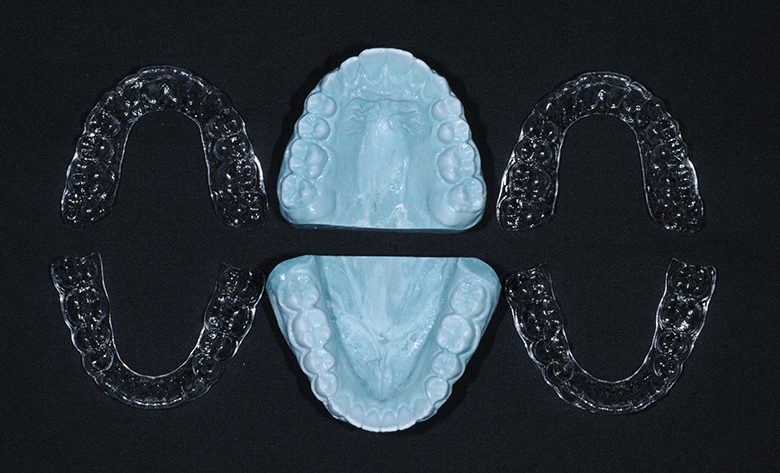
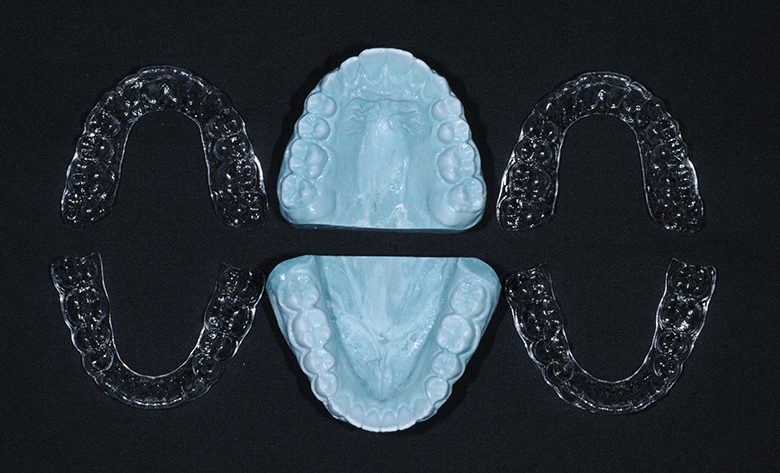
I use the following types of retainers:
Full Coverage Essix Retainers
Essix retainers a re very good at maintaining the entire arch and keeping spaces closed. Upper and lower essix retainers resist wear due to plastic against plastic. Whenever there are natural teeth against essix plastic the retainer will need replacement in as short a time as one year, depending on the grinding habits of the patient. This is why upper and lower essix retainers act as a grinding or bruxing guard and help to cushion the TM joint.
After the braces are removed impressions are taken and two upper and two lower Essix retainers are made in our lab and delivered to the patient on the same day. An appointment is made for one month later. At that appointment final photos are taken and the retainers are checked. The patient is given the models that the retainers were made on so that if a retainer is lost a new one can be made immediately.
It is important that the patient always has two sets of retainers so that if one is lost there is always a backup. The models are made of resin-reinforced stone that resists breakage and allows multiple retainers to be made.
Patients are asked to wear the retainers full time for one week and then every night after that for two years. At that time the patient is given the option of wearing the retainers less but at least two nights per week, or continuing with every night.
Bonded Lingual Retainers
Full coverage Essix retainers are made for all patients to be worn at night, even if they have bonded lingual retainers. This is to retain posterior teeth and closed extraction sites. If a bond fails on a fixed lingual retainer (and they do) the Essix retainer is worn full time to maintain tooth positions until a new lingual retainer is bonded indirectly.




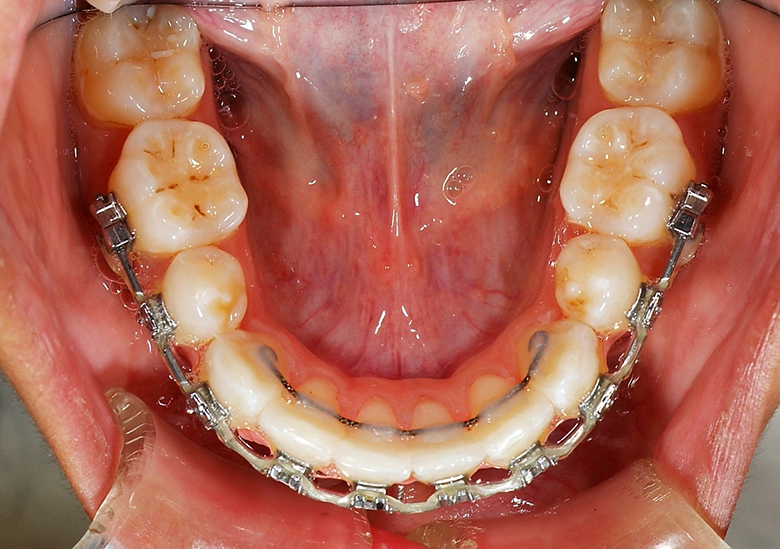
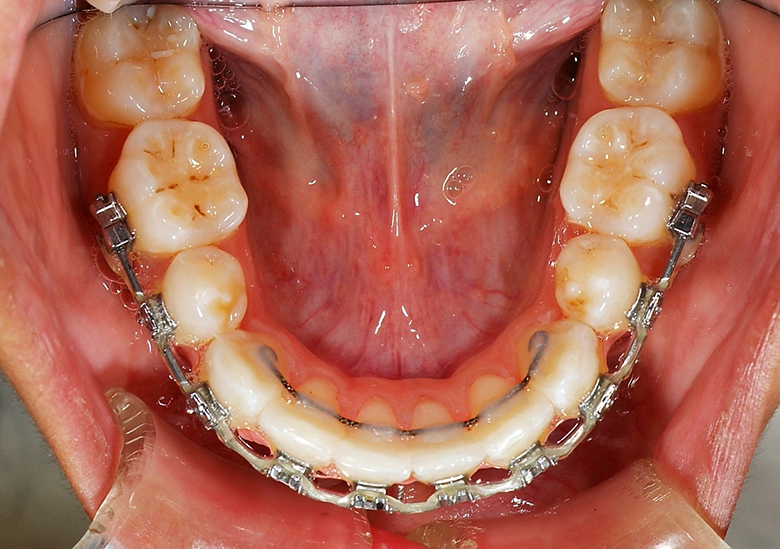


Lingual Retainers Indirect Bonded Before Debond






Lingual Retainer on Model & In Transfer Tray and Lingual Retainer Bonded to Canines Only, Always Combined with a Removable Essix
The Following Articles Reinforce Why I Like Essix Retainers


- Casko J, Shepherd W. Dental and Skeletal Variation Within the Range of Normal. Angle Orthod 1984; 54: 5-17.
- Sameshima GT, Sinclair PM. Predicting and preventing root resorption: part II. Treatment factors. Am J Orthod Dentofacial Orthop 2001;119:511-5.
- Sondhi, Anoop: Efficient and Effective Indirect Bonding. Am J Orthod Dentofacial Orthop 1999;115:352-9.
- Kalange J: Ideal appliance placement with APC brackets and indirect bonding. J Clin Orthod 33:516-526, 1999
- Brin I. Tulloch C. Koroluk L. Philips C. External apical root resorption in Class II malocclusion: A retrospective review of 1- versus 2-phase treatment. Am J Orthod Dentofacial Orthop 2003; 124:151-6.
- Higgins D. Indirect Bonding with Light-Cured Adhesive and a Hybrid Transfer Tray. Semin Orthod 2007;13:64-68.
- Miles P, Weyant R, Rustveld L. A clinical trial of Damon 2 vs conventional twin brackets during initial alignment. Angle Orthod 2006; 76: 480-485.
- Harris D, Jones A, Darendeliler A. Volumetric analysis of root resorption craters after application of controlled intrusive light and heavy orthodontic forces: A microcomputed tomography scan study. Am J Orthod Dentofacial Orthop 2006; 130: 639-647.
- Badawi H, Toogood R, Carey J, Heo G, Major P. Torque expression of self-ligating brackets. Am J Orthod Dentofacial Orthop 2008;133:721-8.
- O'Brien, K et al. Effectiveness of treatment for Class II malocclusion with the Herbst or Twin-block appliances: A randomized, controlled trial. Am J Orthod Dentofacial Orthop 2003;124:128-37.
- Ruf S, Hansen K, Pancherz H. Does orthodontic proclination of lower incisors in children and adolescents cause gingival recession? Am J Orthod Dentofacial Orthop 1998;114.
- Barbagallo L, Jones A, Petocz P, Darendeliler A. Physical properties of root cementum: Part 10. Comparison of the effects of invisible removable thermoplastic appliances with light and heavy orthodontic forces on premolar cementum. A microcomputed-tomography study. Am J Orthod Dentofacial Orthop 2008;133:218-27
- Carlos Flores-Mir, Abenaa Ayeh, Ashim Goswani, Shouresh Charkhandeh. Skeletal and Dental Changes in Class II division 1 Malocclusions Treated with Splint-Type Herbst Appliances.The Angle Orthodontist The Angle Orthodontist Volume 77, Issue 2 (March 2007) pp. 376-381
- Carlos Flores-Mir, Michael P. Major, Paul W. Major. Soft Tissue Changes with Fixed Functional Appliances in Class II division 1. The Angle Orthodontist Volume 76, Issue 4 (July 2006) pp. 712-720
- Carlos Flores-Mir, Paul W. Major. Cephalometric Facial Soft Tissue Changes with the Twin Block Appliance in Class II division 1 Malocclusion Patients. The Angle Orthodontist Volume 76, Issue 5 (September 2006) pp. 876-881
- Sayeh Ehsani, Marie-Alice Mandich, Tarek H. El-Bialy, Carlos Flores-Mir. Frictional Resistance in Self-Ligating Orthodontic Brackets and Conventionally Ligated Brackets. The Angle Orthodontist Volume 79, Issue 3 (May 2009) pp. 592-601
- Amy Archambault, Ryan Lacoursiere, Hisham Badawi, Paul W. Major, Jason Carey, Carlos Flores-Mir. Torque Expression in Stainless Steel Orthodontic Brackets. The Angle Orthodontist Volume 80, Issue 1 (January 2010) pp. 201-210
- Anchalee Paetyangkul, Tamer Türk, Selma Elekdağ-Türk, Allan S. Jones, Peter Petocz, M. Ali Darendeliler. Physical properties of root cementum: Part 14. The amount of root resorption after force application for 12 weeks on maxillary and mandibular premolars: A microcomputed-tomography study. American Journal of Orthodontics & Dentofacial Orthopedics October 2009 (Vol. 136, Issue 4, Pages 492.e1-492.e9)
- Short-term skeletal and dental effects of the Xbow appliance as measured on lateral cephalograms. Carlos Flores-Mir, Gregory Barnett, Duncan W. Higgins, Giseon Heo, Paul W. Major. Am J Orthod Dentofacial Orthop 2009; 136: 822-32
- Three-dimensional orthodontic force measurements. Hisham M. Badawi, Roger W. Toogood, Jason P. R. Carey, Giseon Heo, Paul W. Major. Am J Orthod Dentofacial Orthop 2009;136:518-28
- Lower incisor inclination changes during Xbow treatment according to vertical facial type. Carlos Flores-Mir, Arden Young, Amira Greiss, Matthew Woynorowski, James Peng. Angle Orthod 2010;80:1075–1080.
- Self-ligating vs conventional brackets in the treatment of mandibular crowding: A prospective clinical trial of treatment duration and dental effects. Nikolaos Pandis, Argy Polychronopoulou, Theodore Eliades. Am J Orthod Dentofacial Orthop 2007;132:208-15.
- Orthodontic therapy and gingival recession: a systematic review. Joss-Vassalli I, Grebenstein C, Topouzelis N, Sculean A, Katsaros C: Orthod Craniofac Res 2010;13:127–141.
- Interarch Maxillary Molar Distalization Appliances for Class II Correction. Berkman M, Haerian A, McNamara J. J Clin Orthod 2008;42:35-42.
- Effectiveness of orthodontic treatment with functional appliances on mandibular growth in the short term. Elvira Marsico, Elda Gatto, Maryalba Burrascano, Giovanni Matarese, and Giancarlo Cordasco. Am J Orthod Dentofacial Orthop 2011;139:24-36.
- Treatment effects of the edgewise Herbst appliance: A cephalometric and tomographic investigation. Ryan VanLaecken, Chris A. Martin, Terry Dischinger, Thomas Razmus, Peter Ngane. Am J Orthod Dentofacial Orthop 2006;130:582-93.
- Prediction of lower incisor proclination during Xbow treatment based on initial cephalometric variables. Tehnia Aziz; Usama Nassar; Carlos Flores-Mir
Angle Orthodontist Online, October 2011.
The Xbow® Class II Corrector is protected by the following patents:
US Patent No. 6,168,430 B1
Canadian Patent No. 2,392,021
Australian Patent No. 774128
Taiwan Patent No. 143,056
Herbst is a trademark of Dentaurum, Inc.
APC, Filtek, Forsus, SmartClip, Transbond, and Unitek are trademarks of 3M Company.
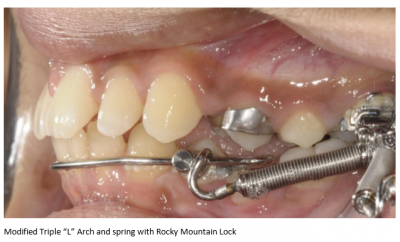
Crossbow, Xbow, Triple "L" Arch and "Straight to the Target When Straight is the Target" are registered trademarks of Dr. Duncan W. Higgins.
Aquarium is a trademark of Dolphin Imaging and Management Solutions.


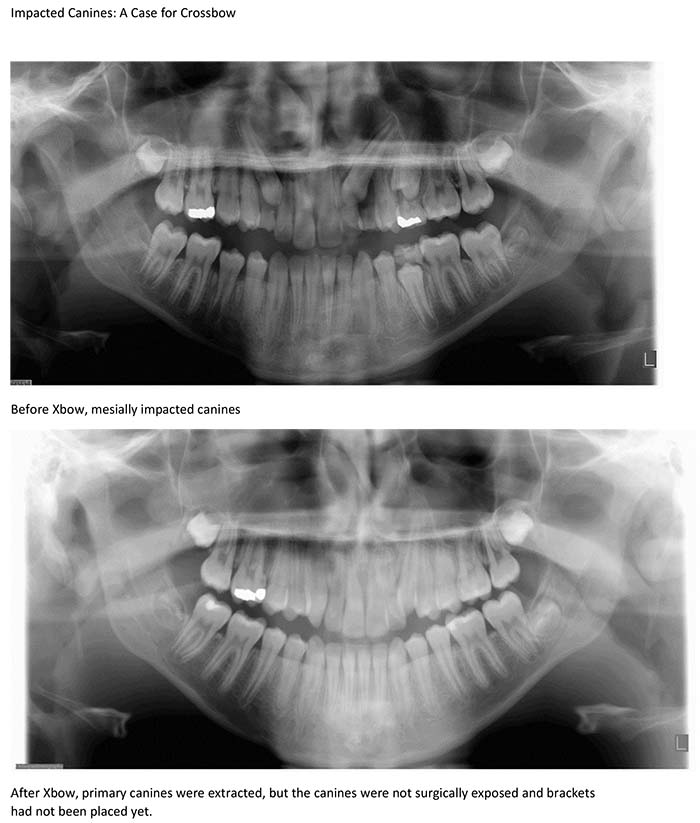
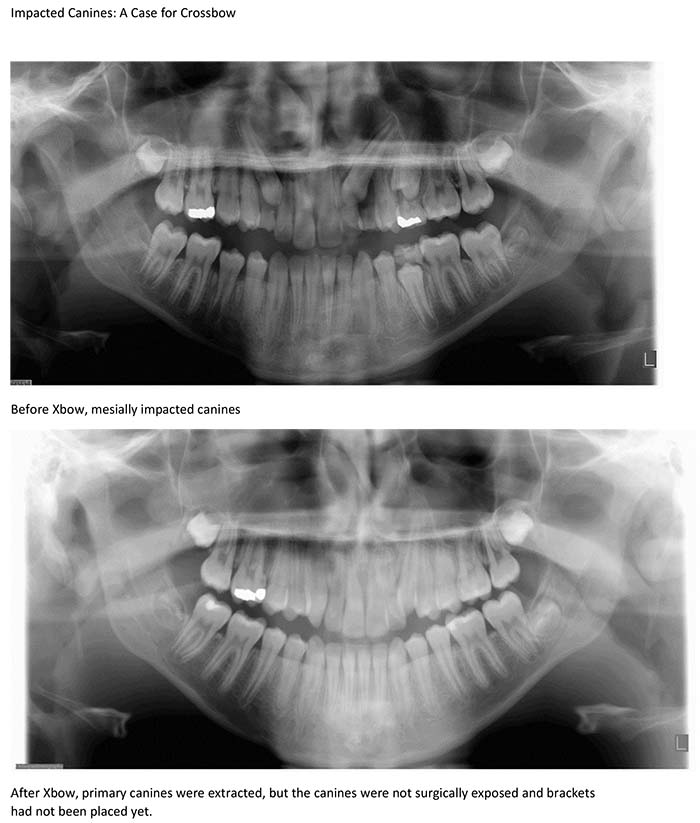
Unilateral Class II: A Case for Crossbow


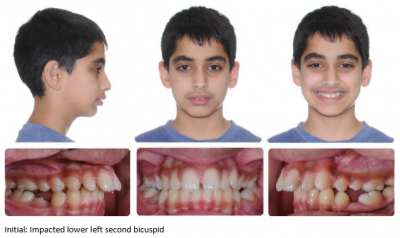
Impacted Lower Second Bicuspid: A Case for Crossbow




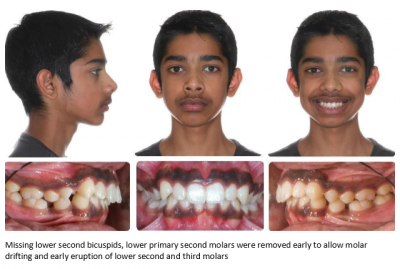
Missing Lower Second Bicuspids: A Case for Crossbow